Crohn’s disease is a chronic and lifelong disorder causing inflammation in the gastrointestinal tract. Although it can involve any part of the GI tract, it commonly affects the small intestine or colon (CCA 2023a).
Crohn’s disease, along with ulcerative colitis, falls under the umbrella of inflammatory bowel disease (IBD) (CCA 2023a).
The severity of Crohn’s disease is unpredictable, but severe flares can lead to hospitalisation and may even require surgery or a temporary or permanent stoma (Healthdirect 2023).
It’s this fluctuating nature of the condition that has the most impact on patients, affecting their emotional, physical and social wellbeing, and causing potentially life-threatening complications (DoH 2019; CCA 2023a).
How Common is Crohn’s Disease in Australia?
Over 100,00 Australians are currently living with inflammatory bowel disease (Better Health Channel 2023), with Australia having one of the highest rates of prevalence in the world (Healthdirect 2023).
As the number of patients with these conditions increases, so too will the cost of treating them.
What is Crohn’s Disease?
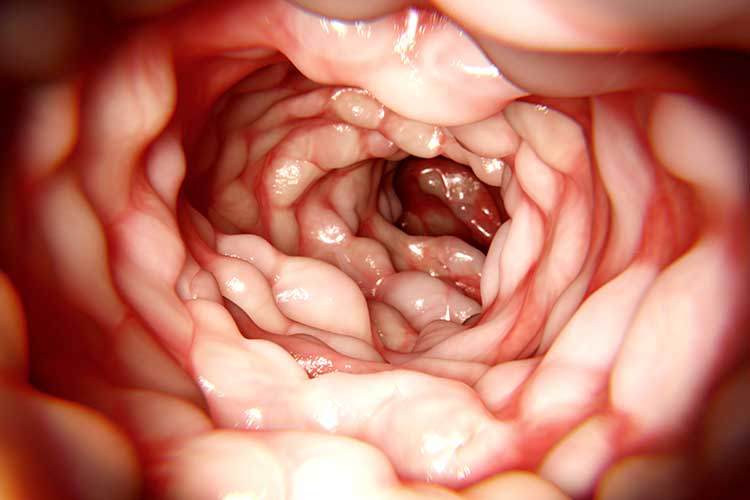
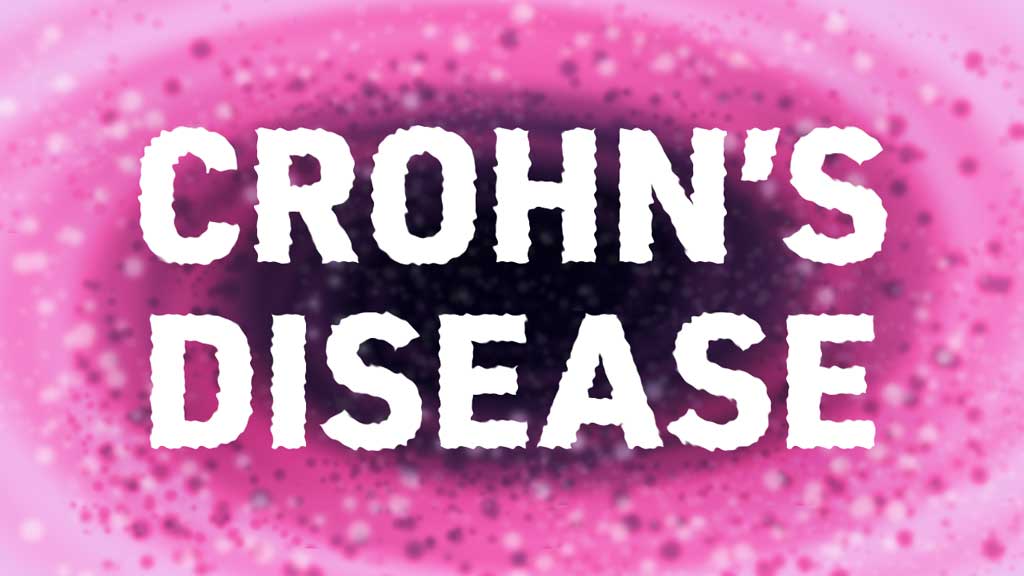
Crohn’s disease causes inflammation in parts of the gastrointestinal tract, often in ‘patches’. Although any part of the GI tract can be affected, including the mouth, oesophagus and stomach, the disease typically begins in the ileum (IBD Clinic 2024).
These patches of inflammation can vary in size, and it’s not unusual for several patches to develop along the GI tract with unaffected sections in between (IBD Clinic 2024).
The inflammation itself can penetrate all layers of the intestinal wall, not just the lining, which can lead to additional complications such as:
- Abscesses and skin tags outside the anus
- Fissures - ulcerated tears/cracks in the lining of the anal canal
- Fistulae - abnormal channels connecting different loops of intestine together, or even to other body organs
- Intestinal obstruction or narrowing of the intestinal wall - known as strictures
- Malabsorption and malnutrition.
(Ranasinghe et al. 2024; Healthdirect 2023)
Symptoms of Crohn’s Disease
Crohn’s disease can affect people of all ages, although symptoms most commonly appear in adolescence and early adulthood (Healthdirect 2023).
Actual symptoms can vary depending on which part of the gut has been affected by the inflammation, but often include diarrhoea, abdominal pain and feeling generally unwell (Healthdirect 2023).
Weight loss is a common feature of Crohn’s disease due to malabsorption and malnutrition, which can also lead to anaemia and vitamin deficiencies. Loss of appetite, fever and fatigue are also frequently seen (Healthdirect 2023; Better Health Channel 2023).
Some less common symptoms that may appear during a Crohn’s flare include:
- Inflammation and pain in the joints
- Uveitis and episcleritis (eye inflammation)
- Liver inflammation
- Skin rashes
- Mouth ulcers.
(CCA 2023b)

How Does Crohn’s Disease Typically Present in Patients?
Crohn’s disease is usually categorised according to the parts of the gut that are most affected by the inflammation.
- Terminal ileal and ileocaecal: Where Crohn’s disease affects the end of the ileum and/or the beginning of the large bowel. This is one of the most common forms of the disease, which typically causes pain in the lower right side of the abdomen, diarrhoea and weight loss.
- Colonic (also known as Crohn’s Colitis): Inflammation is found in the colon. The main symptom here is diarrhoea with blood and mucus. The colon can’t hold as much waste as usual due to the inflammation, and this causes frequent bowel movements.
- Small bowel (also known as ileitis or jejunoileitis, depending on which part of the small bowel is affected): Abdominal pain, diarrhoea and nutrient deficiencies are the common symptoms here, with this form of Crohn’s disease more commonly seen in children and teenagers.
- Perianal: Where inflammation is found in the anus. It’s common for perianal symptoms to develop before intestinal symptoms with this form of Crohn’s disease - for example, anal tags, fissures and fistulas, haemorrhoids and abscesses.
- Gastroduodenal: A much less common form of Crohn’s disease where the inflammation is found in the oesophagus, stomach or duodenum. Typical symptoms include indigestion-type pain, nausea, vomiting, poor appetite, weight loss and anaemia.
(IBD Clinic 2024)
Crohn’s Disease v Ulcerative Colitis
The key difference between Crohn’s disease and ulcerative colitis is that the latter only affects the large intestine, where ulcers and sores will develop. These can then produce mucous and pus, leading to abdominal discomfort, frequent bowel movements and other symptoms (CCA 2023c, d).
Causes of Crohn’s Disease
It’s unknown what exactly causes Crohn’s disease, although it’s likely related to several factors including genetics and triggers to the immune system (e.g. antigens in the environment such as bacteria or viruses) (Healthdirect 2023).
Diagnosing Crohn’s Disease
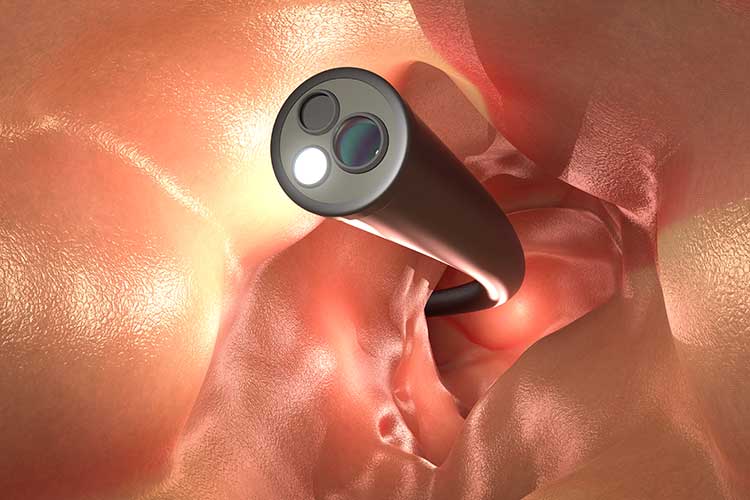
Due to the similarities between Crohn’s disease and other conditions (e.g., ulcerative colitis, and irritable bowel syndrome), it’s important to exclude these other conditions to avoid misdiagnosis (CCA 2022).
Generally, no single test can diagnose Crohn’s disease, so a combination of tests will be used (Healthdirect 2023).
Endoscopy (colonoscopy, sigmoidoscopy or upper GI endoscopy) is often used to examine the colon for signs of inflammation (CCA 2022).
A biopsy might be taken from infected areas of the gut to rule out other possibilities such as infection (Healthdirect 2023).
Other tests used to distinguish between the two types of inflammatory bowel disease include blood tests, stool sample testing and bowel imaging and scans (CCA 2022).
Treatment of Crohn’s Disease
There is no cure for Crohn’s disease, although there are a variety of treatments that can be used to manage the condition and its symptoms. Typically, a holistic approach using medicines, lifestyle management and surgery, where necessary, will be taken (Healthdirect 2023).
Inflammation can be managed using medicines such as steroids, aminosalicylates, immunosuppressants and biologics (Healthdirect 2023).
Monoclonal antibodies can also be used in patients with severe cases of Crohn’s disease where other medicines have failed to make an impact. These are genetically engineered antibodies that block the action of a chemical called cytokine tumour necrosis factor alpha (TNF-α), which is involved in the inflammation process of Crohn’s disease, thereby suppressing the immune system’s response (Tidy & Hazell 2023).
Diet modification can be helpful in reducing and managing symptoms (Better Health Channel 2023).
Individual meal plans are important, as symptoms vary per patient according to where the inflammation is located. An effective meal plan will ensure that essential nutrients aren’t being lost during flare-ups and that nutrition is adequate for the individual and their lifestyle (Fletcher & Luo 2017).
In some cases, where the disease is severe and not responding to medication, or the patient is at risk of colorectal cancer, surgery might be required. A colostomy might also be performed (CCA 2024).
Symptoms of Crohn’s can be unpredictable, and a well-managed case can quickly turn into a severe flare-up of the disease. Frequent communication between the patient and their healthcare practitioners is essential in identifying early symptoms and making rapid referrals when required.
Careful management is essential for this chronic condition.
As Crohn’s disease is a chronic and lifelong condition, it requires careful management from the patient and a good working relationship with the healthcare team around them. Unfortunately, many patients feel disheartened and experience anxiety and depression alongside the condition (Crohn's & Colitis Foundation 2019).
This is particularly common in younger patients, who, while experiencing a flare-up, have been found to experience a lower quality of life and have a higher depression score than those in remission (Brooks et al. 2016).
It’s important to identify risk factors both pertaining to Crohn’s disease and comorbidities that may develop over a patient’s lifetime in order to ensure that the best care is delivered, and adverse complications are reduced and prevented wherever possible.
Test Your Knowledge
Question 1 of 3
Which one of the following treatments is considered a last resort when managing Crohn's disease?
Topics
References
- Better Health Channel 2023, Crohn's Disease and Ulcerative Colitis, Victoria State Government, viewed 20 September 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/crohns-disease-and-ulcerative-colitis
- Brooks, AJ, Rowse, G, Ryder, A, Peach, EJ, Corfe, BM & Lobo, AJ 2016, ‘Systematic Review: Psychological Morbidity in Young People With Inflammatory Bowel Disease – Risk Factors and Impacts’, Alimentary Pharmacology and Therapeutics, vol. 44, no. 1, viewed 23 September 2024, https://onlinelibrary.wiley.com/doi/10.1111/apt.13645
- Crohn's & Colitis Australia 2022, Crohn’s Disease Diagnosis, CCA, viewed 20 September 2024, https://crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease/crohns-disease-diagnosis/
- Crohn's & Colitis Australia 2023a, About Crohn’s Disease, CCA, viewed 20 September 2024, https://crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease/about-crohns-disease/
- Crohn's & Colitis Australia 2023b, Crohn’s Disease Symptoms, CCA, viewed 23 September 2024, https://crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease/crohns-disease-symptoms/
- Crohn's & Colitis Australia 2023c, About Ulcerative Colitis, CCA, viewed 23 September 2024, https://crohnsandcolitis.org.au/about-crohns-colitis/ulcerative-colitis/about-ulcerative-colitis/
- Crohn's & Colitis Australia 2023d, Ulcerative Colitis Symptoms, CCA, viewed 23 September 2024, https://crohnsandcolitis.org.au/about-crohns-colitis/ulcerative-colitis/ulcerative-colitis-symptoms/
- Crohn's & Colitis Australia 2024, Crohn’s Disease Treatment, CCA, viewed 23 September 2024, https://crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease/crohns-disease-treatment/
- Crohn's & Colitis Foundation 2019, Depression and Anxiety, Crohn's & Colitis Foundation, viewed 23 September 2024, https://www.crohnscolitisfoundation.org/mental-health/depression-anxiety
- Department of Health 2019, Inflammatory Bowel Disease National Action Plan 2019, Australian Government, viewed 20 September 2024, https://www.health.gov.au/sites/default/files/documents/2019/09/national-strategic-action-plan-for-inflammatory-bowel-disease-inflammatory-bowel-disease-national-action-plan-2019_0.pdf
- Fletcher, J & Luo, E K 2017, ‘What is the Difference Between Crohn's Disease and Ulcerative Colitis?’, Medical News Today, 6 June, viewed 23 September 2024, https://www.medicalnewstoday.com/articles/317792
- Healthdirect 2023, Crohn's Disease, Australian Government, viewed 20 September 2024, https://www.healthdirect.gov.au/crohns-disease
- IBD Clinic 2024, Crohn's Disease, IBD Clinic, viewed 20 September 2024, http://www.ibdclinic.ca/what-is-ibd/crohns-disease/
- Ranasinghe, IR, Tian, C & Hsu, R 2024, ‘Crohn Disease’, StatPearls, viewed 23 September 2024, https://www.ncbi.nlm.nih.gov/books/NBK436021/
- Tidy, C & Hazell, T 2023, Crohn's Disease, Patient, viewed 23 September 2024, https://patient.info/digestive-health/inflammatory-bowel-disease/crohns-disease
 New
New