What is Prone Ventilation?
The prone position is a body position in which the patient lies flat on their stomach with their limbs unextended. Prone ventilation is the delivery of ventilation to a patient in this position (Biology Dictionary 2019; Malhotra 2024).
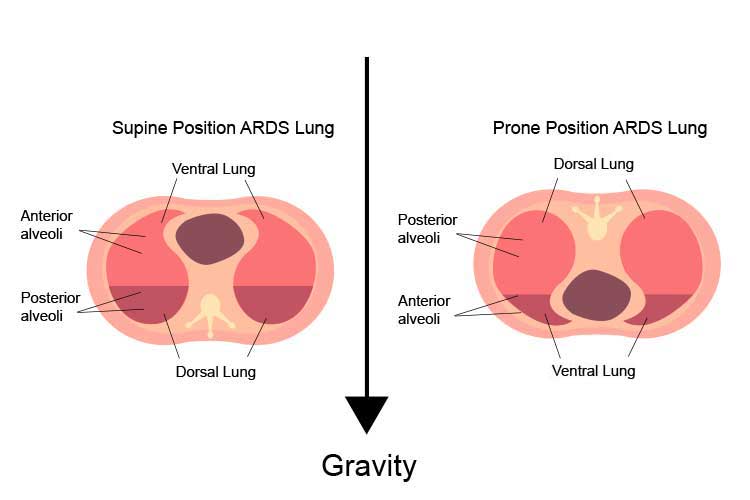
Mechanical ventilation is usually delivered with the patient in the supine position, however, a patient with acute respiratory distress syndrome (ARDS) may be manoeuvred into the prone position to assist with oxygenation when other traditional or advanced modes of ventilation have not been successful (Malhotra 2024).
Prone positioning improves gas exchange by reducing dorsal lung compression and improving lung perfusion. It also assists in moving secretions using gravity to assist in alveoli recruitment and improve oxygenation (Malhotra 2024).
The effects of prone ventilation can include:
- Improved bronchial secretion drainage
- Improved gas exchange (oxygenation)
- Increased alveoli recruitment.
(Yartsev 2024)
Note: Manual prone positioning must always be performed with multiple medical and critical care nurses as it can cause haemodynamic instability whilst turning (Morata & Rechter 2023).
The following article is only intended as a guide. Always refer to your organisation’s policies and procedures for caring for a patient in a prone position.
Skills Needed to Care for a Patient in Prone Position
- Certification as a critical care nurse
- Knowledge (upskilling) about caring for a critically ill patient
- A moderate understanding of the haemodynamic implications of caring for a patient
- A sound understanding of the surrounding critical care environment and equipment in use, such as central venous catheters
- Training in basic life support or advanced life support
- An understanding of airway management principles.
(CICM 2016; Oliveira et al. 2017)
Caring for a Patient in Prone Position
Patients receiving prone ventilation are acutely unwell and will be mechanically ventilated and on life-supporting medicines. All safety measures must be considered along with contingency plans so you are prepared for potential deterioration.
When coming onto a shift to care for a patient who is already in the prone position, the following safety check should be conducted:
- Perform hand hygiene and don personal protective equipment (PPE).
- Bedside handover must be obtained to ensure all care and plans have been communicated to the primary nurse.
- Perform bed safety area checks and patient assessment.
- Locate the emergency trolley in the clinical area.
- Check that oxygen and suctioning are working.
- Perform bag-valve-mask check for ventilating the patient if there are complications with the mechanical ventilator. This acts as a temporary ventilator until the issue has been rectified.
- Head-to-toe assessment must be performed, commencing from the central nervous system. The respiratory system, cardiac system, gastrointestinal system and renal system should be assessed, and a skin integrity check should be performed.
- Assess airway, endotracheal tube placement and ties; ensure mouth care has been performed; check for pressure areas on lips; and ensure the endotracheal tube is moved once per shift to minimise the risk of injury.
- A 5-lead cardiac monitor should be connected to the patient. This may be difficult to see due to the prone positioning. Seek assistance from a fellow clinician to certify lead placement or ensure the cardiac rhythm strip demonstrates correct electrophysiology.
- Ensure non-invasive blood pressure cuff is attached to the patient.
- Ensure the pulse oximeter probe is attached to the patient to ensure continuous monitoring of oxygen saturation. The attachment may be on the finger or forehead. This is vital to ensure the patient's oxygen supply is therapeutic for the patient's condition at all times.
- There should be safe placements of all central venous catheters, arterial catheters, indwelling catheters, nasogastric tubing, drain tubes, continuous venovenous haemofitration (CVVH) and ventilator tubes. They should all be free from potential occlusion. This is important as it could have serious implications if medications and therapies are unable to be delivered, resulting in a medical emergency.
- Check the central venous catheters, arterial line and peripheral line insertion sites for any signs of infection as per hospital protocol (read: How to Assess a Peripheral Intravenous (IV) Cannula).
- Traceback all lines to pumps to ensure the right medication is on the right line. Refer to the hospital’s medication and critical care manuals to ensure there are no medication interactions.
- Ensure lines are all labelled with the correct medication.
- Ensure all lines are free from any occlusion.
- Check mechanical ventilation modes, settings and alarms to ensure the therapy is administered correctly. A ventilator check must be performed with a critically trained clinician, nurse or doctor.
- Perform a safety check of the continuous renal replacement therapy (CRRT) if applicable, to be checked by a critically trained nurse or doctor.
- Pressure area care on a critically ill patient is imperative to ensure all bony prominences are protected to decrease the risk of skin tears, skin breakdown and pressure injuries.
(Morata & Rechter 2023)

Contraindications for Prone Positioning
Contraindications for prone positioning may include:
- Inadequately trained staff
- Spinal or pelvic instability
- Anterior burns or wounds
- Haemodynamic instability
- Raised intracranial or abdominal pressure.
(Yartsev 2024; Nickson 2024)
Possible Complications of Prone Positioning
Though infrequent, the complications of prone positioning can be serious, and the manoeuvre requires skill and teamwork. However, with appropriately trained and experienced staff, these risks are generally mitigated (Oliveira et al. 2017).
You should be aware of the following possible complications:
- Haemodynamic changes: Although prone positioning is beneficial, sometimes it is met by some deterioration:
- In approximately 50% of ARDS patients experiencing haemodynamic instability, the primary cause is right ventricular (RV) failure
- In the remaining cases, haemodynamic compromise is typically attributed to sepsis, which is commonly associated with ARDS.
- Displacement of the endotracheal tube, resulting in hypoxaemia and decrease in ventilation. To protect the airway you must use a bag-valve-mask to deliver oxygen to the patient until help arrives. You can do this by using the facemask attachment and connecting it straight on the endotracheal tube, depending on the situation. If unsure, always call for assistance.
- Arterial blood gases must be obtained to assess the respiratory and metabolic profile when a patient is deteriorating.
- A sputum plug may accumulate in the endotracheal tube. The patient will become hypoxic and require high doses of oxygen and immediate medical treatment. The patient must have a humidification circuit applied to ensure patency of the tube at all times. Humidification must always be applied at the commencement of mechanical ventilation to decrease sputum plugs.
- Hypoxia: You may need to increase oxygen therapy and ventilate the patient with a bag-valve-mask and call for medical assistance.
- Medication lines occluding: You should traceback lines and identify the issue, and ask for help if patient haemodynamics are declining.
- The patient may be in cardiac arrest. CPR must commence immediately on the patient when in a prone position to optimise blood flow and perfuse vital organs. You must refer to the protocols from your workplace.
(DePasse et al. 2015; Zou et al. 2017; Vieillard-Baron et al. 2023)
Always Remember...
- Ensure all bed safety checks are carried out
- Perform a thorough head-to-toe assessment
- Call for assistance when a patient deteriorates
- Treat the signs and symptoms of the patient (e.g. if the patient's oxygen saturations are decreasing and hypoxic, give oxygen to the patient).
Test Your Knowledge
Question 1 of 3
What is the first thing you should do after you receive a bedside handover?
Topics
Further your knowledge
References
- Biology Dictionary 2019, Prone Position, Biology Dictionary, viewed 17 April 2025, https://biologydictionary.net/prone-position/
- College of Intensive Care Medicine of Australia and New Zealand 2016, Minimum Standards for Intensive Care Units, CICM, viewed 28 April 2025, https://www.cicm.org.au/common/Uploaded%20files/Assets/Accredited%20Sites/Unit%20Seeking%20Accreditation/IC-1-Minimum-Standards-for-Intensive-Care-Units.pdf
- DePasse, J, Palumbo, MA, Haque, M, Eberson, CP & Daniels, AH 2015, ‘Complications Associated with Prone Positioning in Elective Spinal Surgery’, World J Orthop., vol. 6 no. 3, viewed 28 April 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4390897/
- Koulouras, V, Papathanakos, G, Papathanasiou, A & Nakos, G 2016, ‘Efficacy of Prone Position in Acute Respiratory Distress Syndrome Patients: A Pathophysiology-based Review’, World J Crit Care Med., vol. 5, no. 2, viewed 17 April 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4848155/
- Malhotra, A 2024, Prone Ventilation for Adult Patients with Acute Respiratory Distress Syndrome, UpToDate, viewed 17 April 2025, https://www.uptodate.com/contents/prone-ventilation-for-adult-patients-with-acute-respiratory-distress-syndrome#H16
- Morata, L & Rechter, J 2023, ‘Manual Prone Positioning in Adults: Reducing the Risk of Harm Through Evidence-Based Practices’, Critical Care Nurse, vol. 43, no. 1, viewed 28 April 2025, https://aacnjournals.org/ccnonline/article/43/1/59/31964/Manual-Prone-Positioning-in-Adults-Reducing-the
- Nickson, C 2024, Prone Position and Mechanical Ventilation, Life in the Fast Lane, viewed 28 April 2025, https://litfl.com/prone-position-and-mechanical-ventilation/
- Oliveira, VM, Piekala, DM, Deponti, CN et al. 2017, ‘Safe Prone Checklist: Construction and Implementation of a Tool for Performing the Prone Maneuver’, Rev Bras Ter Intensiva., vol. 29, no. 2, viewed 28 April 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5496747/
- Vieillard-Baron, A, Boissier, F & Pesenti, A 2023, ‘Hemodynamic Impact of Prone Position. Let’s Protect the Lung and its Circulation to Improve Prognosis’, Intensive Care Medicine, vol. 49, viewed 28 April 2025, https://link.springer.com/article/10.1007/s00134-023-07001-2
- Yartsev, A 2024, Prone Ventilation for ARDS, Deranged Physiology, viewed 17 April 2025, https://derangedphysiology.com/main/required-reading/mechanical-ventilation/Chapter-517/prone-ventilation-ards
- Zou, W, Shao, J, Li, L, He, Z & Guo, Q 2017, ‘A Randomized Comparison of the Prone Ventilation Endotracheal Tube Versus the Traditional Endotracheal Tube in Adult Patients Undergoing Prone Position Surgery’, Sci Rep., viewed 28 April 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5431779/
 New
New