Throughout history, pulmonary embolism (PE) has almost always been diagnosed on the autopsy table. In other words, it was considered a ‘terminal event’ (Doherty 2017).
Today, PE is seen as a modern-day medical dichotomy: we understand its minutia and yet, somehow, still fail to diagnose or tackle it appropriately.
Appropriately treated, pulmonary embolism need not live up to its historical reputation as a life-ender.
What is a Pulmonary Embolism?
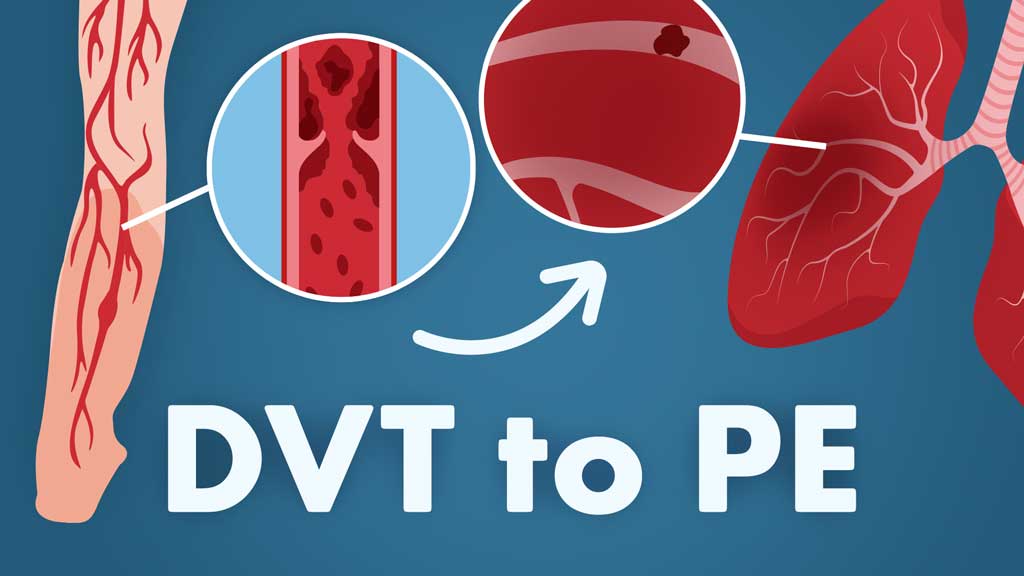
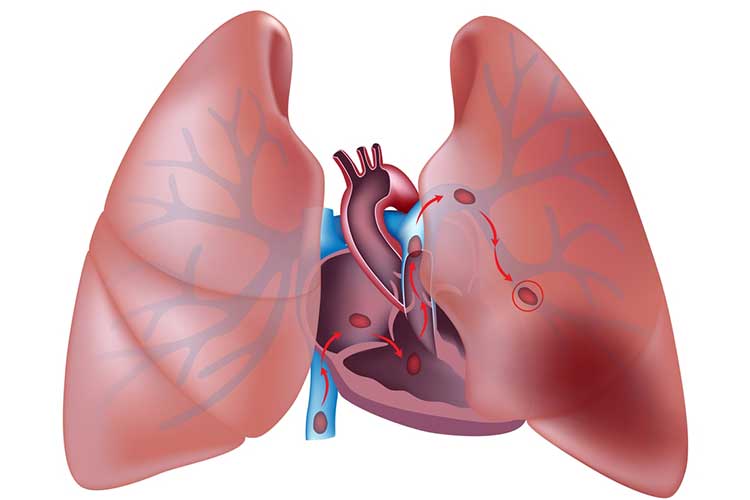
Pulmonary embolism (PE) is a natural consequence of a cascade of unfortunate events that begin with a thrombus formation, typically in a deep vein of the legs, thighs or pelvis (Fig. 1).
With venous thromboembolism events, where there is smoke, there is usually fire. Three risk factors, collectively described as Virchow's triad, are the ‘smoke’ that occurs prior to a PE diagnostic fire.
Virchow’s Triad
Virchow's triad consists of:
- Hypercoagulability (blood disorders that increase the risk of clotting), for example, an inherited Factor V Leiden mutation
- Abnormal blood flow, for example, stasis due to obesity or immobility
- Vessel wall injury (aka endothelial Injury), for example, damage from smoking or sepsis.
(Garmo et al. 2023; Kushner et al. 2024; Ausmed 2021)
The presence of these risk factors places patients at a significantly elevated risk of the venous event turning into a much bigger pulmonary problem.
In fact, over 50% of patients with deep venous thrombi will eventually end up with a diagnosis of PE (Stevens et al. 2024).
Causes of Pulmonary Embolism
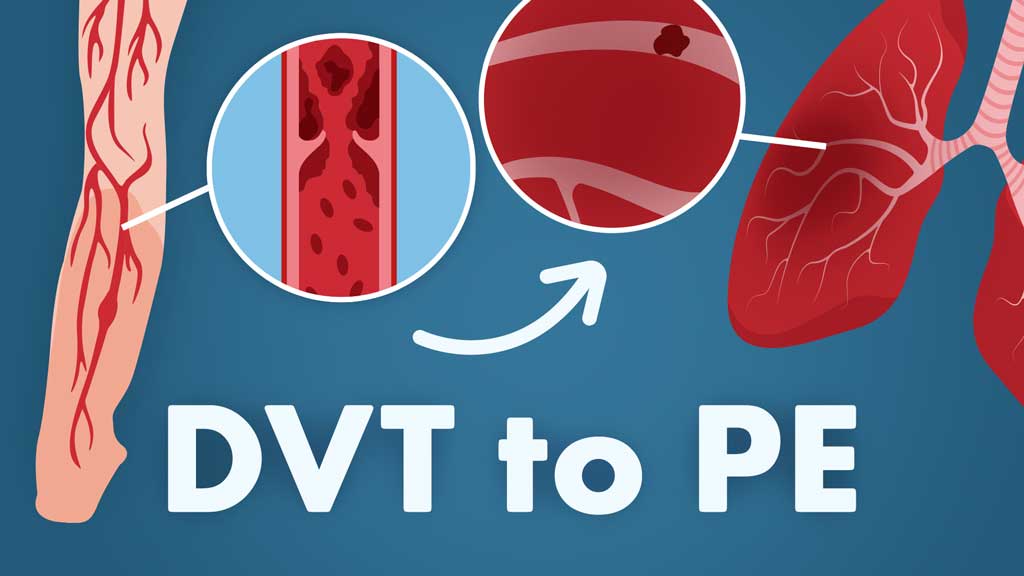
DVTs can be caused by anything that prevents normal circulation in the legs, including bed rest or limited movement, injury, bracing, surgery, or even certain types of medicines (see risk factors for more info).
DVTs are largely preventable, which means that PEs are also largely preventable.
Patients who maintain a healthy weight, exercise (or at least do not maintain a sedentary lifestyle) and follow directions related to post-surgery care or bedrest are far less likely to develop a DVT.
The most prominent signs of a DVT are:
- Redness or discolouration
- Swelling
- Warmth in the affected area
- Pain, especially a cramping sensation in the calf (Fig. 2).
(Mayo Clinic 2022a)
A Homans’ sign is no longer considered a sensitive or specific test for DVT (Lin et al. 2024).

Symptoms of Pulmonary Embolism
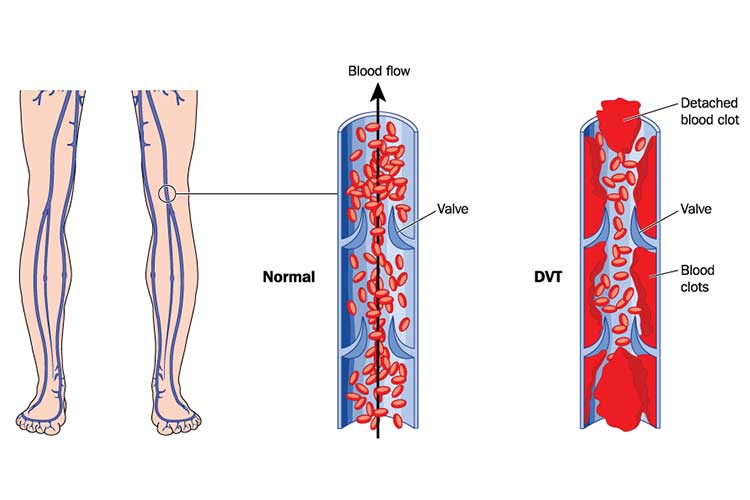
Pulmonary embolism typically begins with the migration of a thrombus formation (Fig. 3), usually from the deep veins of the leg to the small blood vessels of the lungs. The clot lodges in these smaller pathways and blocks blood flow, potentially leading to tissue death.
It is important to know that patients can experience a PE without any prior symptoms of a DVT.
The most common signs and symptoms of PE include:
- Dyspnoea (laboured breathing)
- Pleuritic chest pain
- Cough
- Haemoptysis (coughing up blood)
- Changes in consciousness.
(Vyas et al. 2024)
Risk Factors for Pulmonary Embolism
Risk factors for DVT (and thus for PE) include many events that tend to lead to injuries to the venous structures of the leg, thigh, hip or pelvis.
Fractures, surgery and significant muscle tears are all conditions that create the potential for DVT formation.
Individuals with slow blood flow have an elevated risk; this flow problem can be due to prolonged sitting from long car rides or aeroplane flights, bed rest, or paralysis.
Pregnancy, hormone replacement therapy and contraceptive medicines are also major culprits due to a common theme: they cause an increase in oestrogen to be delivered to the body.
Central venous catheters must be closely monitored.
Even certain medical conditions such as cardiopulmonary disease, inflammatory bowel conditions and obesity can increase the risk.
Certainly, a family history of DVT or PE or any type of genetic clotting disorder will also elevate the odds.
These odds increase further in older adults.
Pulmonary Embolism Diagnosis and Testing
The diagnostic strategy for PE should depend on clinical probability (Boka et al. 2024).
Over time, clinicians have developed working models to determine the probability of a PE diagnosis. There are many available, but the Wells model is easy to use and well-established.
Wells’ Score for Clinical Prediction
| Active cancer (patient receiving treatment for cancer within 6 months or currently receiving palliative treatment) | +1 |
| Haemoptysis | +1 |
| History of deep venous thrombosis or pulmonary embolism | +1.5 |
| Immobilisation for at least three days OR surgery within the past four weeks | +1.5 |
| Heart rate > 100 beats/min | +1.5 |
| Pulmonary embolism judged to be the most likely diagnosis | +3 |
| Clinical signs and symptoms compatible with deep venous thrombosis | +3 |
- A score of less than 2 indicates a low probability of PE
- A score of 2-6 indicates an intermediate probability of PE
- A score of more than 6 indicates a high probability of PE.
(Vyas et al. 2024)
The Pulmonary Embolism Rule-out Criteria
The Pulmonary Embolism Rule-out Criteria (PERC) is used to rule out PE only in cases where the pre-test probability of PE is less than 15% (Medscape 2020).
According to the PERC rule, PE can be ruled out in a patient who presents with NONE of the following characteristics:
- Age ≥50
- Heart rate ≥ 100 beats/min
- Oxygen saturation < 95% on room air
- Unilateral leg swelling
- Haemoptysis
- Surgery or trauma within the past four weeks
- History of PE or DVT
- Oestrogen use.
(Medscape 2020)
If the patient has at least one of the above characteristics, then PE cannot be ruled unlikely without further assessment (Medscape 2020).
Further Testing
Computed tomographic pulmonary angiography (CTPA) is the standard diagnostic imaging tool used to determine the presence of a PE (Fig. 4). This test allows clinicians to visualise the small vessels of the lungs using a contrast dye injected into a vein.
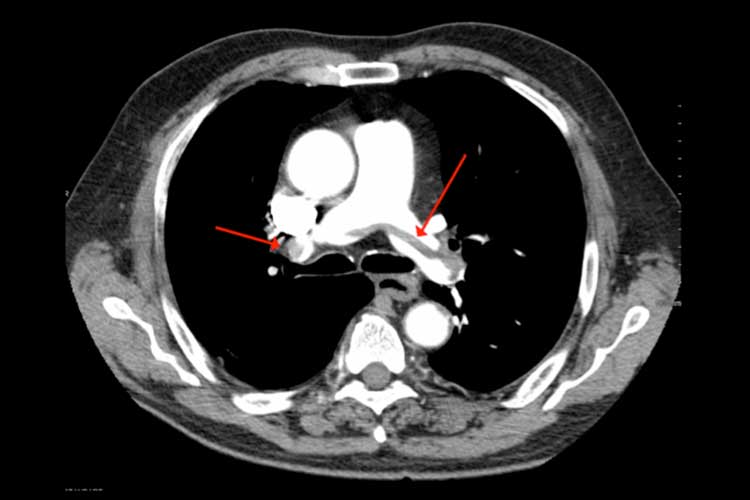
Patients with a high probability of PE (based on the criteria above) should immediately undergo a CTPA, which will either confirm or refute the presence of a PE (Vyas et al. 2024).
To reduce unnecessary imaging, patients with a low or moderate probability of PE should undergo a D-dimer test (preferably with a highly sensitive assay) (Boka et al. 2024).
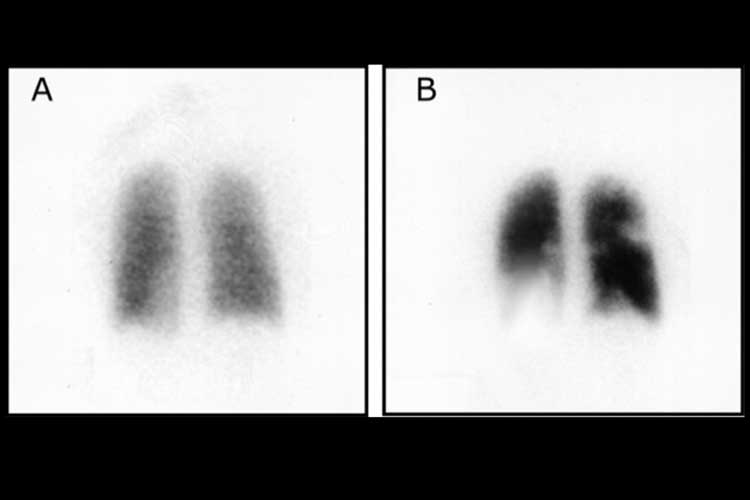
Other tests, such as ventilation-perfusion (V/Q) scans (Fig. 5) and pulmonary angiography, can also be used to diagnose PE (Vyas et al. 2024).
Treating Pulmonary Embolism
The first-line treatment for most patients with PE is direct oral anticoagulants (DOACs) (Dix & Tran 2022).
Anticoagulants are often referred to as ‘blood thinners’, but this is not actually what they do. Instead, they reduce the ability of blood to clot, allowing the body time to reduce the size of the clot by reabsorption. They also make it less likely that the blood will clot again in the near future.
Patients with PE will typically receive anticoagulant therapy for 3-6 months (Dix & Tran 2022).
Thrombolytics, which work to dissolve clots, are recommended for severely compromised patients with a systolic blood pressure of < 90 mmHg (Doherty 2017).
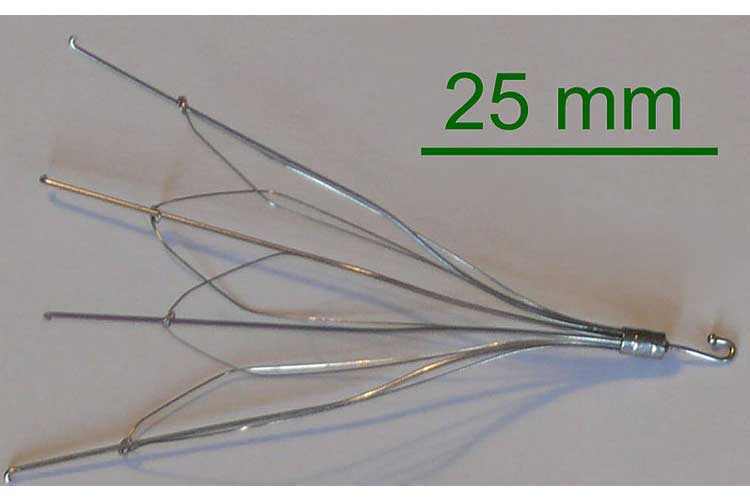
A vena cava filter (Fig. 6) can be placed in the inferior vena cava to prevent clots from migrating from the legs into the lungs. However, this treatment is only indicated in certain situations, including when anticoagulant therapy is absolutely contraindicated (Vyas et al. 2024).
Embolectomy is a procedure used to remove a clot surgically.
Complications of Pulmonary Embolism
Untreated PE has a mortality rate of 30% (Vyas et al. 2024).
Major complications include:
- Recurrent thromboembolism
- Chronic thromboembolic pulmonary hypertension (CTEPH)
- Right heart failure
- Cardiogenic shock.
(Vyas et al. 2024)
One of the most severe complications, chronic thromboembolic pulmonary hypertension (CTEPH), is associated with a high risk of death. It’s estimated to occur in up to 5% of post-PE patients but may be underdiagnosed due to initial nonspecific symptoms (Sabbula et al. 2024; Fedullo 2024).
Preventing Pulmonary Embolism
PE, although serious, can be prevented when appropriate measures are taken.
The first step to prevent PE is becoming aware of the risk. If you are at an increased risk, a doctor can recommend medicines or graduated compression stockings to help prevent a DVT from occurring (Fig. 7).
The risk of PE also increases when sitting for extended periods of time. This can be mitigated by getting up to walk, wearing loose-fitting clothes while travelling and exercising your legs while seated.
Stretching your leg muscles by lifting your heels off the ground and setting them down again is a good way to do this. Finally, maintaining a healthy weight and active lifestyle is key to reducing the risk of PE (Mayo Clinic 2022b).
Conclusion
Pulmonary embolism is a potentially preventable condition. It is also potentially life-ending.
As already discussed, the best clinical outcome is when the embolism never makes it to the lungs. The best way to prevent the embolism from migrating to the lungs is to prevent it from ever forming in the lower extremities in the first place.
Clinician management of PE has changed over the years, with many excellent tools available to clinicians to allow them to bypass unnecessary tests and delay times.
With PE, time management is the most important treatment tool of them all.
Test Your Knowledge
Question 1 of 3
A patient who underwent surgery within the past four weeks is experiencing haemoptysis. Using the Wells’ Score for Clinical Prediction, what is the probability of pulmonary embolism for this patient?
Topics
Further your knowledge
 Free
Free Free
Free Free
Free
References
- Ausmed Editorial Team 2021, ‘An Introduction to Blood Clots’, Ausmed, 19 May, viewed 22 July 2024, https://www.ausmed.com.au
- Boka, K, Ouellette, DR, Harrington, A, Kamangar, N & Soo Hoo, GW 2024, Pulmonary Embolism Clinical Scoring Systems, Medscape, viewed 22 July 2024, https://emedicine.medscape.com
- Department of Health and Aged Care 2021, Reducing Clot Complications, Australian Government, viewed 22 July 2024, https://www.health.gov.au
- Dix, C & Tran, H 2022, ‘Pulmonary Embolus’, Australian Journal of General Practice, vol. 51, no. 9, viewed 22 July 2024, https://www1.racgp.org.au
- Doherty, S 2017, ‘Pulmonary Embolism: An Update’, Australian Family Physician (Chest Pain), vol. 46, no. 11, viewed 22 July 2024, https://www.racgp.org.au
- Fedullo, P 2024, Epidemiology, Pathogenesis, Clinical Manifestations and Diagnosis of Chronic Thromboembolic Pulmonary Hypertension, UpToDate, viewed 22 July 2024, https://www.uptodate.com
- Garmo, C, Bajwa, T & Burns, B 2023, ‘Physiology, Clotting Mechanism’, StatPearls, viewed 22 July 2024, https://www.ncbi.nlm.nih.gov
- Kushner, A, West, WP, Khan Suheb, MZ & Pillarisetty, LS 2024, ‘Virchow Triad’, StatPearls, viewed 22 July 2024, https://www.ncbi.nlm.nih.gov
- Lin, JL, Shin, RD & Brenner, BE 2024, Deep Venous Thrombosis (DVT), Medscape, viewed 22 July 2024, https://emedicine.medscape.com
- Medscape 2020, PERC Rule for Pulmonary Embolism, Medscape, viewed 22 July 2024, https://reference.medscape.com
- Mayo Clinic 2022a, Deep Vein Thrombosis (DVT), Mayo Clinic, viewed 22 July 2024, https://www.mayoclinic.org
- Mayo Clinic 2022b, Pulmonary Embolism, Mayo Clinic, viewed 22 July 2024, https://www.mayoclinic.org
- Stevens, S, Woller, SC & Fontaine, GV, ‘Pulmonary Embolism’, BMJ Best Practice, viewed 22 July 2024, https://bestpractice.bmj.com
- Sabbula, B, Sankari, A & Akella, J 2024, ‘Chronic Thromboembolic Pulmonary Hypertension’, StatPearls, viewed 22 July 2024, https://www.ncbi.nlm.nih.gov
- Vyas, V, Sankari, A & Goyal, A 2024, ‘Acute Pulmonary Embolism’, StatPearls, viewed 22 July 2024, https://www.ncbi.nlm.nih.gov
 New
New