What are Learning Communities of Practice?
Learning Communities of Practice are groups of people who share a concern, a set of problems, or a passion about a topic, and who deepen their knowledge and expertise in this area by interacting on an ongoing basis (Wenger, McDermott, & Snyder, 2002). These communities develop a shared repertoire of resources: experiences, stories, tools, and ways of addressing recurring problems – in short, a shared practice. This shared repertoire enables community members to effectively tackle challenges and innovate within their field, fostering a culture of continuous learning and improvement.
What is the Role of Learning Communities of Practice in Australian Healthcare Education?
Learning Communities of Practice in Australian healthcare serve as a vital mechanism for knowledge management, bridging the gap between theory and practice. They support the Australian healthcare system by promoting continuous professional development, enhancing the quality of health services, and facilitating the integration of health information and health insurance policies into practice. In this way, they contribute significantly to the improvement of patient care and healthcare outcomes.
Examples of Learning Communities of Practice in Healthcare
Examples include interdisciplinary teams of medical specialists, allied health professionals, and primary care providers who collaborate to improve patient care. These communities foster an environment where members engage in shared learning experiences, contributing to the advancement of healthcare practices. By working together, these groups help to break down silos within the healthcare system, encouraging a more holistic and patient-centred approach to care.
How to Build a Learning Community of Practice?
Building a Learning Community of Practice involves several steps, starting from identifying the shared interest or challenge among potential members to facilitating ongoing engagement and knowledge sharing. It requires commitment from community members and support from the healthcare organisation to thrive. Establishing a successful community also depends on creating a safe and open environment where members feel valued and empowered to share their insights and experiences.
Steps to Build Learning Communities of Practice in Healthcare
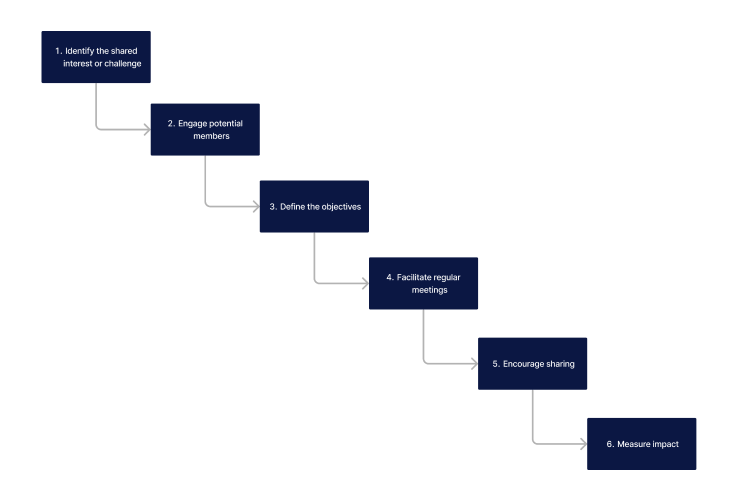
Prior to listing the steps, it's essential to understand that the success of a Learning Community of Practice hinges on the active participation and engagement of its members. These communities thrive on the diversity of their members' experiences, which enriches the learning and development process for all involved.
- Identify the shared interest or challenge: Among health professionals to foster a sense of common purpose.
- Engage potential members: Determine their needs and interests to guide the objectives of the community
- Define the objectives: Ensure alignment with broader organisational goals and member's goals.
- Facilitate regular meetings: Reinforce interactions among members to encourage ongoing dialogue and collaboration.
- Encourage sharing: Promote a culture of open communication and mutual support whereby members can share their experiences, resources, and best practices.
- Measure impact: Review the community's impact on professional practice and patient care to demonstrate value and identify areas for improvement.
What are the Benefits and Negatives of Learning Communities of Practice in Healthcare?
While inclusive learning programs offer numerous advantages for healthcare education, they also present certain challenges that need to be managed effectively.
| Benefits | Negatives |
|---|---|
| Enhanced professional development and lifelong learning. | Time constraints may limit participation and engagement. |
| Improved patient outcomes through shared best practices. | Resource limitations can affect the community's activities and growth. |
| Stronger healthcare system with collaborative problem-solving. | Varying levels of engagement among members can impact community dynamics. |
| Increased innovation in healthcare practices. | Potential for information overload, leading to disengagement. |
| Development of a supportive network for health professionals. | Challenges in maintaining long-term momentum and interest. |
| Facilitation of interdisciplinary collaboration and understanding. | Difficulty in aligning individual and group objectives. |
| Creation of a repository of shared knowledge and resources. | Technological barriers may hinder access and participation for some members. |
| Promotion of a culture of continuous improvement and critical thinking. | Risks of conflicts or disagreements due to diverse viewpoints. |
Tips for Implementing Learning Communities of Practice
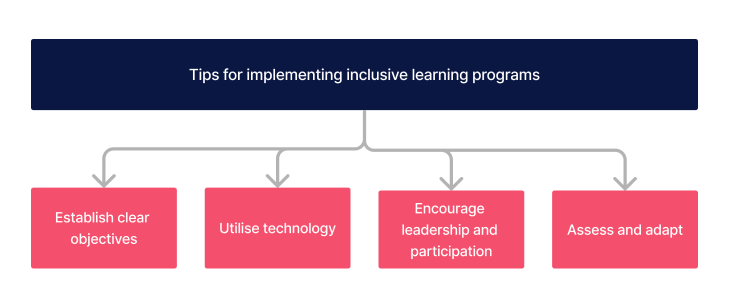
Effective utilisation of Learning Communities of Practice involves more than just bringing people together. It requires strategic actions to ensure that the community's activities are meaningful and impactful.
- Establish clear objectives and expectations for community members to guide their interactions and contributions.
- Utilise technology to facilitate communication and knowledge sharing, making it easier for members to connect and collaborate.
- Encourage leadership and active participation from all members, recognizing and valuing the diverse skills and perspectives they bring.
- Regularly assess and adapt the community's activities based on feedback, ensuring that it remains relevant and responsive to members' needs.
Need an LMS that supports your communities of practice?
Contact Ausmed today and see how we can support your organisation!
Tools to Design Learning Communities of Practice
Selecting the right tools is crucial for fostering effective communication, collaboration, and knowledge sharing within Learning Communities of Practice. Here are some key technologies that can support these communities:
- Learning Management Systems (LMS): Platforms that provide a structured environment for sharing educational content, facilitating discussions, and managing community activities.
- Online Forums: Dedicated forums or message boards offer spaces for in-depth discussions, problem-solving, and exchange of ideas among community members.
- Social Media Groups: Platforms such as LinkedIn groups or Facebook pages can help in connecting members, sharing quick updates, and fostering a sense of community.
- Video Conferencing Tools: Tools like Zoom or Microsoft Teams enable virtual meetings, workshops, and real-time discussions, crucial for communities spread across different locations.
- Collaborative Document Platforms: Google Docs, Microsoft OneDrive, and similar platforms allow members to collaboratively work on documents, policies, and resources in real-time.
- Project Management Tools: Applications like Trello, Asana, or Slack can help in organizing community projects, tracking progress, and ensuring tasks are completed efficiently.
Related Resources
- Mandatory Training: How an LMS can help you meet requirements
- LMS in Healthcare: The Roles, Benefits and Pros and Cons
- LMS in Disability Care: The Roles, Benefits and Pros and Cons
- What Is the Role of an LMS in Aged Care?
- How to Create a Culture of Continuous Learning
- How to Manage an Effective Staff Training Program
- How Can I Use Peer Feedback to Enhance Learning?
- 360-Degree Feedback in Learning and Development
- How Can I Implement Self-Directed Learning Strategies?
Conclusion
Learning communities of practice represent a powerful approach to fostering inclusive and effective learning environments in the healthcare sector. By leveraging the collective knowledge and experience of community members, healthcare organisations can enhance the quality of care, support professional development, and navigate the complexities of the healthcare system more effectively. As such, they play a crucial role in the ongoing development of healthcare professionals and the improvement of healthcare services.
References
- Wenger, E., McDermott, R., & Snyder, W.M. (2002). Cultivating communities of practice: A guide to managing knowledge. Harvard Business Press.
- Li, SA., Jeffs, L., Barwick, M. and Stevens, B., 2018. 'Organizational contextual features that influence the implementation of evidence-based practices across healthcare settings: a systematic integrative review', Systematic Reviews, 7(1), p.72. Available at: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-018-0734-5
- Ranmuthugala, G., Plumb, J.J., Cunningham, F.C., Georgiou, A., Westbrook, J.I. and Braithwaite, J., 2011. 'How and why are communities of practice established in the healthcare sector? A systematic review of the literature', BMC Health Services Research, 11, p.273. Available at: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-11-273



