In the fast-paced and ever-evolving world of healthcare, the need for a robust and dynamic approach to professional development is critical. This is where the concept of a competency framework becomes invaluable. It acts as a comprehensive guide to help healthcare education and learning managers systematically identify, develop, and nurture the essential skills and knowledge required in the healthcare sector. This extended article delves deeper into the concept of a competency framework, its pivotal role in healthcare, and the methodologies to construct an effective one, with a special focus on adaptive learning strategies and the utilisation of appropriate tools.
What is a Competency Framework?
A competency framework is an organisational tool that outlines the specific skills, knowledge, and behaviors necessary for effective performance in various roles within an organisation. In healthcare, this involves detailing core competencies critical for different positions, from primary care to urgent care and long-term aged care. These competencies encompass not just technical skills but also interpersonal attributes and decision-making capabilities.
Why are Competency Frameworks Important to Healthcare?
Competency frameworks in healthcare serve multiple critical functions. They help bridge skills gaps, guiding health professionals in their career development and ensuring they possess the competencies required to deliver high-quality care. In the context of mental health, for instance, these frameworks provide clarity on the skills needed for effective patient care, which can vary significantly from other healthcare sectors. Moreover, they aid in performance management, ensuring that staff across all levels are competent in their roles, which is essential for the delivery of safe and efficient health services.
Examples of 'Competency Frameworks'
Several competency frameworks have been developed and implemented across various sectors in healthcare, each tailored to meet the specific needs of different disciplines and roles. Some notable examples include:
Nursing Competency Frameworks:
- Royal College of Nursing (RCN) Framework: Specifically designed for mental health nurses, focusing on skills essential for mental health care.
- Emergency Nursing Competency Framework: Outlining the competencies needed for nurses in emergency settings, including crisis management and urgent care skills.
Medical Practitioners Competency Frameworks:
- General Practitioner (GP) Framework: Covering competencies required for general practitioners in areas like patient communication, diagnosis, and treatment planning.
- Specialist Competency Frameworks: For various specialties such as cardiology, oncology, etc., highlighting specialized skills and knowledge needed in these areas.
Healthcare Administration Frameworks:
- Health Services Management Framework: Concentrating on competencies for healthcare administrators, including leadership, financial management, and policy implementation.
- Healthcare Information Management Framework: Focused on skills necessary for managing healthcare information systems and data privacy.
Allied Health Professionals Frameworks:
- Physical Therapy Competency Framework: Detailing the skills and knowledge needed for physical therapists, including patient assessment and rehabilitation techniques.
- Occupational Therapy Framework: Outlining competencies for occupational therapists, focusing on patient rehabilitation and daily living skills improvement.
Mental Health and Social Care Frameworks:
- Mental Health Counselor Framework: Targeting competencies required for mental health counselors, including patient empathy, crisis intervention, and therapy techniques.
- Social Worker Competency Framework: Focusing on skills needed for social workers in healthcare settings, such as patient advocacy, community resource management, and family support systems.
Long-term and Aged Care Frameworks:
- Aged Care Nursing Framework: Designed for nurses working in aged care, covering competencies like geriatric assessment, palliative care, and dementia care.
- Long-term Care Management Framework: Focusing on skills needed for managing long-term care facilities, including patient care coordination and facility administration.
Each of these frameworks is designed to guide the training, assessment, and professional development of healthcare workers in their respective fields, ensuring that they are equipped with the necessary skills and knowledge to provide high-quality care.
How to Build a Competency Framework for Skill Development
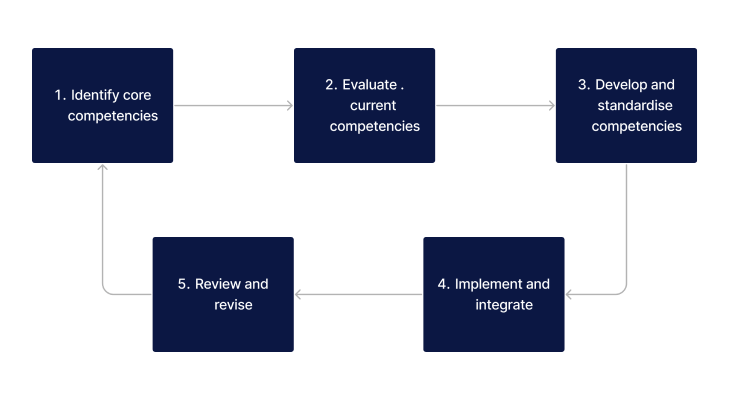
Building an effective competency framework involves several key steps:
- Identify Core Competencies: This involves consulting with various stakeholders, including healthcare practitioners, patients, and regulatory bodies, to determine the essential skills and knowledge for different roles.
- Evaluate Current Competencies: Assess the current skill levels of healthcare professionals to identify any gaps in knowledge or abilities.
- Develop and Standardise Competencies: Establish clear, measurable standards for each identified competency.
- Implement and Integrate: Apply the framework across various functions, such as hiring, training, and performance evaluations.
- Review and Revise: Regularly update the framework to reflect technological advancements, policy changes, and evolving healthcare needs.
Want a healthcare LMS that can support staff meeting your competency frameworks?
Contact Ausmed today and see how we can support your organisation!
Considerations When Using 'Competency Frameworks' in Healthcare
When implementing competency frameworks in healthcare, there are several key considerations to ensure their effectiveness and relevance:
| Consideration | Explanation |
|---|---|
| Alignment with Healthcare Goals | Ensure the competency framework aligns with the overall goals and values of the healthcare system. This includes considering patient care standards, healthcare policies, and industry regulations. |
| Inclusivity and Diversity | The framework should be inclusive, accommodating the diverse range of roles within healthcare, from direct patient care providers to administrative and support staff. This diversity ensures comprehensive development across all sectors of healthcare. |
| Stakeholder Engagement | Engage a wide range of stakeholders, including healthcare professionals, educators, and policy makers, in the development of the framework. This ensures that it reflects the actual needs and challenges of the healthcare environment. |
| Flexibility and Scalability | The framework should be flexible enough to accommodate changes in healthcare practices, technology, and policies. It should also be scalable to different sizes and types of healthcare organisations. |
| Practicality and Relevance | Ensure that the competencies included are practical and directly relevant to the roles for which they are intended. The framework should be a useful tool for both learning and application in real-world healthcare settings. |
| Ongoing Evaluation and Revision | Regularly evaluate and update the framework to ensure it remains current and effective. This includes monitoring its impact on healthcare delivery and professional development. |
| Integration with Professional Development | The framework should be integrated with existing professional development programs and continuing education initiatives. This helps in ensuring that the competencies are not only learned but also applied and reinforced over time. |
| Support and Resources | Provide adequate support and resources for the implementation of the framework. This includes training for educators and managers, as well as tools and materials for learners. |
| Measuring Effectiveness | Develop metrics and evaluation methods to assess the effectiveness of the competency framework in improving skills, knowledge, and overall healthcare delivery. |
| Cultural Competence | Include competencies that promote cultural competence, ensuring that healthcare professionals are equipped to provide care that is respectful of and responsive to the health beliefs, practices, and needs of diverse patients. |
By considering these factors, healthcare organisations can effectively implement and utilise competency frameworks to enhance professional development, improve patient care, and respond to the dynamic needs of the healthcare sector.
Tools to Build Competency Frameworks for Skill Development
To effectively build and implement a competency framework, various tools can be utilised:
- Learning Management Systems (LMS): These digital platforms are essential for delivering educational content, tracking learner progress, and identifying areas for improvement.
- Competency Mapping Tools: Tools that help in mapping out the required competencies for different roles and identifying the existing skills within the workforce.
- Feedback and Evaluation Tools: Instruments such as 360-degree feedback mechanisms that provide comprehensive insights into the competencies and performance of healthcare professionals.
Related Resources
- LMS in Healthcare: The Roles, Benefits and Pros and Cons
- Mandatory Training: How an LMS can help you meet requirements
- Guide to Mandatory Training
- Mandatory Training in Aged Care (A Guide for Managers)
- Adapting to Regulatory Changes in Healthcare Training
- Policy Management: A Guide for Healthcare Managers
- Guide to Compliance Training (for Healthcare Managers)
- A Guide to Creating Your Own Training Modules
Conclusion
The development of a competency framework in healthcare is an intricate and ongoing process. It necessitates an in-depth understanding of the unique dynamics of the healthcare sector, the identification and nurturing of core competencies, and the effective integration of adaptive learning strategies. By leveraging the right tools and methodologies, education and learning managers can construct a robust and effective competency framework, fostering a culture of continuous professional development and excellence in healthcare.
References
- RACGP. (n.d.). The Clinical Competencies for the CCE. Retrieved from www.racgp.org.au
- ACHSM. (n.d.). Health Service Management Competency Framework. Retrieved from achsm.org.au
- Psychotherapy and Counselling Federation of Australia (PACFA). (n.d.). National minimum standards for counselling and psychotherapy. Retrieved from pacfa.org.au