Cellulitis is a common but potentially serious condition with ‘unacceptably high’ hospitalisation rates (ACSQHC 2021).
What is Cellulitis?

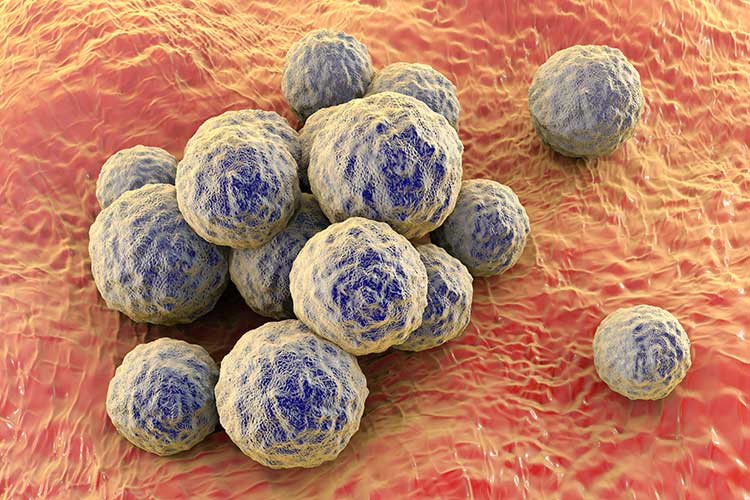
Cellulitis is an infection of the subcutaneous tissue and skin, leading to inflammation and other systemic symptoms (Healthdirect 2023). It’s caused by bacteria, with the most common causative pathogens being:
(Better Health Channel 2023)
Rarely, cellulitis may be caused by:
- Pseudomonas aeruginosa
- Haemophilus influenzae
- Anaerobes, Eikenella or Streptococcus viridans
- Pasteurella multocida
- Vibrio vulnificus
- Aeromonas hydrophila
- Erysipelothrix.
(Stanway et al. 2016)
Cellulitis is common but has the potential to become life-threatening if left untreated (Mayo Clinic 2022). In fact, prior to the invention of antibiotics, it was a fatal condition (Better Health Channel 2023).
What Causes Cellulitis?
Cellulitis occurs when bacteria enter the body and spread to the subcutaneous tissue, generally through a break in the skin caused by inflammation or damage (Better Health Channel 2023).
Skin areas prone to cellulitis infection include:
- Insect or animal bites
- Burns
- Abrasions, cuts, bruises or grazes
- Ulcers
- Surgical wounds
- Skin conditions (e.g. eczema, psoriasis, scabies, acne, tinea, chickenpox/shingles)
- Tattoos or piercings
- Penetrating trauma.
(Better Health Channel 2023; ACSQHC 2021; NHS Inform 2025; CDC 2024)
Despite this, bacteria can also enter the body through undamaged skin, and in many cases, a specific cause cannot be identified (Better Health Channel 2023).
Risk Factors for Cellulitis
- Damaged skin areas (see above)
- Lymphoedema
- Obesity (which causes poorer circulation)
- Diabetes
- Chronic liver or kidney disease
- Pre-existing skin infections (e.g. tinea)
- Mobility issues
- Weakened immune system (e.g. due to chemotherapy)
- Pregnancy
- Injection drug use
- Smoking
- Alcohol abuse
- Previous cellulitis infection
- Crowded living conditions
- Socioeconomic disadvantage.
(ACSQHC 2021; NHS 2024; Better Health Channel 2023; Stanway et al. 2016)
Symptoms of Cellulitis

The primary symptom of cellulitis is inflamed skin in the affected area. It may appear red, painful, swollen, sensitive and/or warm (Healthdirect 2023). The infected area may also leak pus or fluid (Better Health Channel 2023).
While any part of the body can be affected (including the face), most cellulitis infections occur in the lower leg (Healthdirect 2023).
If the infection spreads, the patient may experience systemic symptoms such as:
- Fever
- Chills
- Sweating
- Nausea and vomiting
- General malaise
- Pain.
(Healthdirect 2023; Better Health Channel 2023)
Complications of Cellulitis
In severe cases, cellulitis may lead to serious complications that require urgent care, such as:
- Necrotising fasciitis
- Gas gangrene
- Sepsis, which may then cause:
- Hypotension
- Reduced capillary circulation
- Heart failure
- Diarrhoea
- Gastrointestinal bleeding
- Renal failure
- Loss of consciousness
- Infection of other organs (e.g. pneumonia, osteomyelitis, meningitis)
- Endocarditis
- Bacteraemia
- Thrombophlebitis.
(Stanway et al. 2016; CDC 2024)
How is Cellulitis Treated?
Cellulitis is generally treated using oral antibiotics, but in cases where there are two or more symptoms of systemic infection, antibiotics are administered intravenously instead (ACSQHC 2021).
Patients should be encouraged to elevate the affected area to assist with drainage, reduce swelling and alleviate pain. Analgesics such as paracetamol may also be taken to relieve symptoms (Better Health Channel 2023).
Most patients will begin to show improvement after two to three days on antibiotics and will fully recover within a week (Better Health Channel 2023).
In more severe cases, surgical intervention may be required (Better Health Channel 2023).
Cellulitis and Hospitalisation
Cellulitis is the fifth most common cause of potentially preventable hospitalisation in Australia and one of the two biggest causes of potentially preventable hospitalisation in Aboriginal and Torres Strait Islander people (AIHW 2024; Aboriginal and Torres Strait Islander Health Performance Framework 2025).
Those who are more likely to be admitted to hospital for cellulitis are:
- Aboriginal and Torres Strait Islander people
- Older, frail people
- People with certain comorbidities (e.g. diabetes, obesity, heart failure)
- People living in crowded conditions
- People who are experiencing socioeconomic disadvantage.
(ACSQHC 2021)
Why Might People With Cellulitis be Hospitalised?
One likely reason for high cellulitis hospitalisation rates is the prevalence of community-associated methicillin-resistant Staphylococcus aureus (MRSA) (strains of S. aureus that have developed antibiotic resistance) in regional and remote communities.
A high prevalence of MRSA increases the likelihood of cellulitis hospitalisation due to:
- Certain antibiotics being ineffective on MRSA strains
- The need for surgical drainage of MRSA infections, which typically requires hospital care
- Increased rates of MRSA-associated skin abscesses, furuncles and boils that may progress to cellulitis.
(ACSQHC 2021)
Other factors that may contribute to cellulitis hospitalisation, as well as differences between hospitalisation rates in different geographical locations, include:
- Diagnostic error (under-diagnosis or over-diagnosis)
- High rates of diabetes, particularly among Aboriginal and Torres Strait Islander people
- Poorly managed diabetes
- High rates of obesity, chronic venous stasis, impaired mobility and lymphoedema
- High rates of streptococcal infections among Aboriginal and Torres Strait Islander people
- Crowded housing
- Use of swimming facilities
- Occupational risk factors for injuring the skin
- High density of people who are more prone to cellulitis (e.g. aged care facilities)
- High temperatures and humidity, which are associated with open footwear and tinea
- Delayed or inadequate access to healthcare
- Poor health literacy
- Lack of access to dermatologists
- Lack of access to culturally appropriate healthcare for Aboriginal and Torres Strait Islander people
- Lack of integrated care that refers patients to social services and programs.
(ACSQHC 2021)
How Can We Reduce Hospitalisation for Cellulitis?
In order to reduce hospitalisation rates, earlier and more appropriate management of cellulitis is required (ACSQHC 2021).
Strategies suggested by the Atlas include:
- Addressing the social determinants of skin health (e.g. crowded living conditions)
- Improving the prevention and management of chronic conditions that may lead to cellulitis
- Improving access to services (e.g. podiatry, lymphoedema management)
- Improving the accuracy of diagnosis
- Consulting with infectious diseases specialists or dermatologists early in the course of the condition
- Using community models of care instead of inpatient care in hospitals
- Promoting skin health among Aboriginal and Torres Strait Islander people
(ACSQHC 2021)
Test Your Knowledge
Question 1 of 3
What kind of infection is cellulitis?
Topics
Further your knowledge
 Free
Free
 Free
Free
References
- Aboriginal and Torres Strait Islander Health Performance Framework 2025, 3.07 Selected Potentially Preventable Hospital Admissions, Australian Government, viewed 13 January 2025, https://www.indigenoushpf.gov.au/measures/3-07-selected-potentially-preventable-hospital-adm
- Australian Commission on Safety and Quality in Health Care 2021, Fourth Australian Atlas of Healthcare Variation 2021, Australian Government, viewed 13 January 2025, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/fourth-australian-atlas-healthcare-variation-2021
- Australian Institute of Health and Welfare 2024, Potentially Preventable Hospitalisations in Australia by Small Geographic Areas, 2020–21 to 2021–22, Australian Government, viewed 13 January 2025, https://www.aihw.gov.au/reports/primary-health-care/potentially-preventable-hospitalisations-2020-22/contents/summary
- Better Health Channel 2023, Cellulitis, Victoria State Government, viewed 13 January 2025, https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/cellulitis
- Centers for Disease Control and Prevention 2024, About Cellulitis, U.S. Department of Health and Human Services, viewed 13 January 2025, https://www.cdc.gov/group-a-strep/about/cellulitis.html
- Healthdirect 2023, Cellulitis, Australian Government, viewed 13 January 2025, https://www.healthdirect.gov.au/cellulitis
- Mayo Clinic 2022, Cellulitis, Mayo Clinic, viewed 13 January 2025, https://www.mayoclinic.org/diseases-conditions/cellulitis/symptoms-causes/syc-20370762
- NHS Inform 2025, Cellulitis, National Health Service Scotland, viewed 13 January 2025, https://www.nhsinform.scot/illnesses-and-conditions/skin-hair-and-nails/cellulitis
- National Health Service 2024, Cellulitis, NHS, viewed 13 January 2025, https://www.nhs.uk/conditions/cellulitis/
- Stanway, A, Gomez, J & Oakley, A 2016, Cellulitis, DermNet NZ, viewed 13 January 2025, https://dermnetnz.org/topics/cellulitis/
 New
New 
