Bleeding disorders affect over 7,000 people in Australia (Haemophilia Foundation Australia 2023a).
The most common bleeding disorders, von Willebrand disease and haemophilia, appear to be similar but have several key differences.
What Are Bleeding Disorders
Bleeding disorders are a group of chronic conditions that occur when proteins in the blood known as clotting factors are absent or dysfunctional (Doherty & Kelley 2023).
As a result, the blood can't clot normally when the person is injured, leading to excessive bleeding (Doherty & Kelley 2023).
For more information on the physiology of blood clots, see the Ausmed Article An Introduction to Blood Clots.
Types of Bleeding Disorders
The three most common bleeding disorders are:
- Von Willebrand disease
- Haemophilia A (factor VIII deficiency)
- Haemophilia B (factor IX deficiency).
(Doherty & Kelley 2023)
Von Willebrand Disease
Von Willebrand disease (VWD) is the most common bleeding disorder around the world, affecting people of all genders and racial backgrounds (Better Health Channel 2022a).
The disorder is caused by an absent or dysfunctional von Willebrand factor (VWF), which slows or impairs the blood clotting process. Consequently, bleeding takes longer to stop than in the average person (Better Health Channel 2022a).
There are three types of VWD:
- Type 1 is the most common and (generally) mildest form of VWD
- Type 2 occurs when there are normal levels of VWF in the body, but it doesn’t work properly. Type 2 VWD is further categorised into one of four subtypes of type 2 (2A, 2B, 2M and 2N), depending on the specific dysfunction.
- Type 3 is the rarest and most severe. It occurs when there is very little to no VWF in the blood.
(Better Health Channel 2022a; CDC 2023)
Causes of Von Willebrand Disease
VWD is almost always an inherited disorder (CDC 2023).
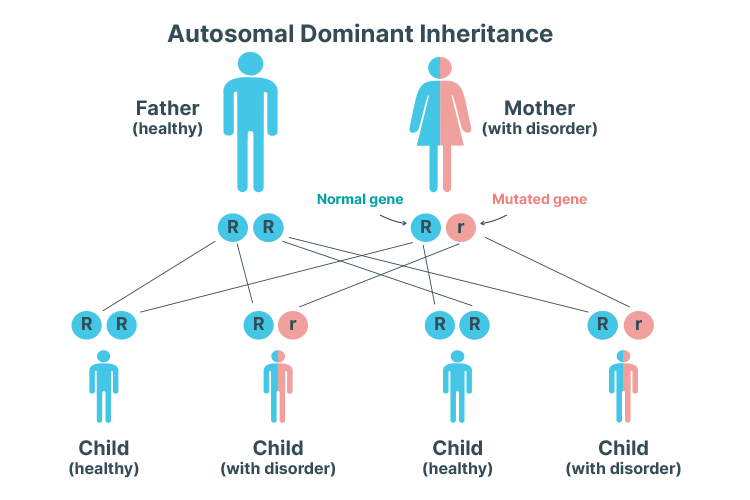
Types 1, 2A, 2B, and 2M are autosomal dominant disorders, meaning that only one parent needs to pass on the mutated gene (i.e. VWD allele) in order for their child to inherit the condition. In other words, the child has a 50% chance of inheriting the disorder, depending on whether they inherit the affected parent’s normal gene or the VWD allele (CDC 2023).
If both parents have VWD, there is a 25% chance of the child inheriting both VWD alleles. In this case, the disorder will be more severe (CDC 2021).
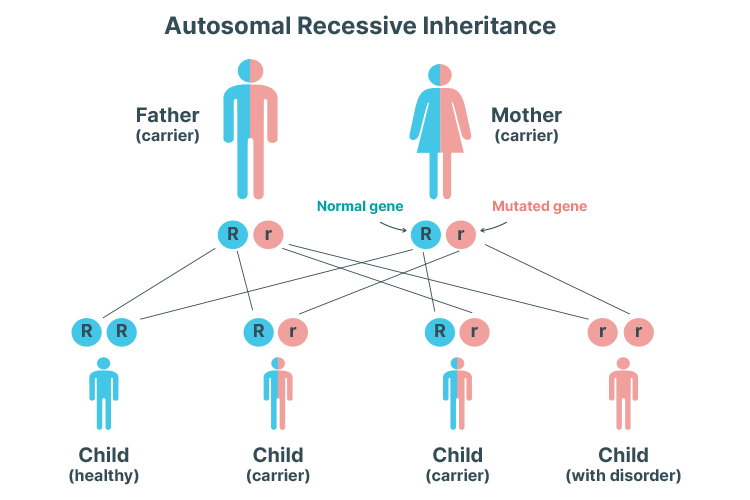
Types 2N and 3, on the other hand, are autosomal recessive disorders, meaning that both parents need to pass on the VWD allele in order for their child to inherit the condition. Therefore, if only one parent has VWD, it’s not possible for the child to inherit the condition - but they might still be a carrier. If both parents have VWD, there’s a 25% chance of the child inheriting the condition (CDC 2023).
In rare cases, the VWF gene can spontaneously mutate, causing VWD even without a family history of the disorder (CDC 2023).
It’s also rare but possible for VWD to be acquired later in life. This is thought to be caused by an autoimmune reaction that destroys the body’s VWF, triggered by illness or certain medicines. This type of VWD is not genetic (CDC 2023).
Symptoms of Von Willebrand Disease
In VWD, bleeding generally affects the mucous membranes (nose, mouth, uterus, vagina, stomach, and intestines) (Better Health Channel 2022a).
Some people with mild illness have no noticeable symptoms and may not even be aware that they have the disorder (Healthdirect 2020).
Symptomatic people might experience:
- Frequent or long-lasting nosebleeds that may occur without injury, last for more than 10 minutes and/or require packing or cautery
- Frequent and easy bruising
- Heavy or prolonged menstrual bleeding - this is often the most significant indicator of the disorder in women
- Excessive bleeding after injury, surgery, childbirth, or dental procedures
- Bleeding from the gum
- Blood in urine or stools
- Spontaneous bleeding episodes, in severe cases
- Bleeding into joints or internal organs, in severe cases.
(CDC 2023; Healthdirect 2020; Doherty & Kelley 2023)

Diagnosing Von Willebrand Disease
Milder cases of VWD may not be recognised until a major bleeding problem occurs and indicates that something is abnormal (e.g. after surgery or an injury) (Better Health Channel 2022a).
Diagnosis might take into account:
- Patient history (e.g. history of bleeding and bruising easily)
- Family history of excessive bleeding
- Specialised laboratory blood tests to detect VWD
- Genetic testing.
(Better Health Channel 2022a)
Routine blood tests may display normal results as VWF levels naturally due to factors such as stress, exercise, and hormones. Therefore, testing may need to be repeated (Better Health Channel 2022a).
Treating Von Willebrand Disease
VWF can’t be cured, but an interprofessional team will help to develop a treatment plan and assist the patient to live well with the disorder (Better Health Channel 2022a).
Treatment options depend on the individual and the severity of their illness but may include:
- Desmopressin - a synthetic hormone that causes the body to release stored VWF and factor VIII into the bloodstream.
- Clotting factor concentrate made with von Willebrand factor (VWF) and factor VIII (FVIII) to replace missing VWF and FVIII in the blood. It’s injected intravenously into the arm and is used when the patient requires treatment for more than two or three days or if desmopressin is contraindicated.
- Tranexamic acid or aminocaproic acid, which help to prevent blood clots from dissolving after being formed.
- Fibrin glue, which can be applied directly to an injury.
- Hormone treatments (e.g. oral contraceptives) to assist with heavy menstrual bleeding and increase levels of VWF and factor VIII.
(Better Health Channel 2022a)
Those with mild illness may only require treatment when undergoing surgery or if injured (Better Health Channel 2022a).
Haemophilia
Haemophilia is a bleeding disorder that occurs when there isn’t enough of either the VIII or IX clotting factor, meaning the blood can’t clot properly (Better Health Channel 2019a). There are two types of haemophilia:
- Haemophilia A, also known as classical haemophilia, is caused by a mutation in the F8 gene and causes factor VIII deficiency
- Haemophilia B, also known as Christmas Disease, is caused by a mutation in the F9 gene and causes factor IX deficiency.
(Better Health Channel 2022b; Haemophilia Foundation Australia 2023b)
Generally, those with less than 40% of the normal level of the clotting factor are considered to have haemophilia (Haemophilia Foundation Australia 2023b).
Most people with haemophilia are male, and severe disease in females is very rare (Haemophilia Foundation Australia 2023b).
Causes of Haemophilia
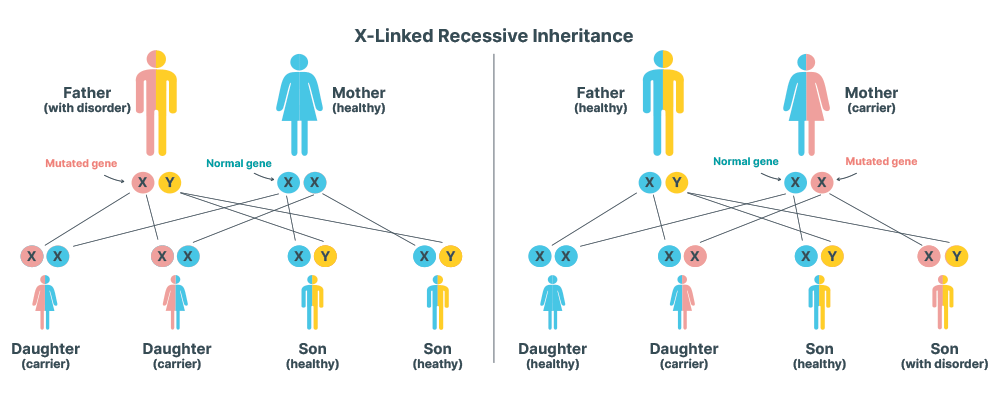
Haemophilia is an X-linked recessive disorder, meaning the mutated gene is on the X chromosome. Males will receive the Y chromosome from their father and either one of their mother’s two X chromosomes. If the mother is a carrier of the mutated haemophilia gene, there is a 50% chance of the male child inheriting the mutation. As males only have one X chromosome, there is no other gene to cancel out the mutation if it is passed on (Centre For Genetics Education 2021).
As females have two X chromosomes, the second X chromosome will generally ‘cancel out’ the mutation (as the mutation is recessive) and therefore, most females who inherit the mutated gene are unaffected or only experience a mild reduction in the affected clotting factor. They will become carriers, however (Haemophilia Foundation Australia 2023c).
This X-linked recessive pattern causes haemophilia to be much more common in males - it affects about 1 in 6,000 to 10,000 males compared to less than 1 per 300,000 females (RCHM 2023).
In about one-third of cases, the gene mutation occurs spontaneously without any family history of the disorder (Haemophilia Foundation Australia 2023c).
Like VWD, it’s possible, but rare, for haemophilia to be acquired later in life (Better Health Channel 2022b).
Classification of Haemophilia
Haemophilia is categorised as either mild, moderate, or severe, depending on the concentration of the affected clotting factor in the patient’s blood:
Note: The typical unaffected person has a concentration of between 50 and 150% factor VIII and factor IX in their blood (Better Health Channel 2022b).
| Severity | Concentration of clotting factor | Characteristics |
|---|---|---|
| Mild | 5 to 40% |
|
| Moderate | 1 to 5% |
|
| Severe | Less than 1% |
|
(Adapted from Better Health Channel 2022b; RCHM 2023)
Symptoms of Haemophilia
Unlike VWD, which predominantly affects the mucous membranes, haemophilia mainly causes internal bleeding into the joints and muscles. This can cause permanent damage over time, potentially leading to arthritis or chronic pain (Better Health Channel 2022b).
Other symptoms may include:
- Easy bruising
- Excessive bleeding following surgery, trauma or childbirth
- Heavy menstrual bleeding.
(Healthdirect 2023)

Signs of haemophilia in early infancy may include:
- Internal bleeding or abnormal swelling or bruising after delivery
- Excessive bleeding after a heel prick or vaccination
- Easy bruising
- Painful swelling
- Reluctance to use a particular arm or leg.
(Better Health Channel 2022b)
Diagnosing Haemophilia
Haemophilia may be diagnosed prenatally, during infancy or later in life. Milder cases of haemophilia might not be diagnosed until the individual undergoes surgery or experiences trauma, as there is often enough of the clotting factor present for minor injuries to heal normally (Better Health Channel 2022b).
Diagnosis may involve:
- Physical indications of unusual bleeding activity
- Family history of excessive bleeding
- Blood tests to check clotting factor levels
- Genetic testing
- Prenatal genetic testing.
(Better Health Channel 2022b)
Treating Haemophilia
Symptoms may be managed similarly to VWD, using treatment options such as:
- Desmopressin
- Clotting factor concentrates
- Tranexamic acid
- Fibrin glue
- Hormone treatments.
(Better Health Channel 2022b)
Test Your Knowledge
Question 1 of 3
True or false: Von Willebrand disease predominantly affects the mucous membranes.
Topics
References
- Better Health Channel 2022b, Haemophilia, Better Health Channel, viewed 1 February 2022, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/haemophilia
- Better Health Channel 2022a, Von Willebrand Disease, Victoria State Government, viewed 29 January 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/von-willebrand-disease
- Centers for Disease Control and Prevention 2023, Von Willebrand Disease (VWD), U.S. Department of Health & Human Services, viewed 29 January 2024, https://www.cdc.gov/ncbddd/vwd/index.html
- Centre For Genetics Education 2021, Fact Sheet 09: X-Linked Recessive Inheritance, New South Wales Government, viewed 29 January 2024, https://www.genetics.edu.au/publications-and-resources/facts-sheets/fact-sheet-9-x-linked-recessive-inheritance
- Doherty, TM & Kelley, A 2023, ‘Bleeding Disorders’, StatPearls, viewed 29 January 2024, https://www.ncbi.nlm.nih.gov/books/NBK541050/
- Haemophilia Foundation Australia 2023a, Fast Facts, Haemophilia Foundation Australia, viewed 29 January 2024, https://www.haemophilia.org.au/about-bleeding-disorders/fast-facts
- Haemophilia Foundation Australia 2023b, Haemophilia, Haemophilia Foundation Australia, viewed 29 January 2024, https://www.haemophilia.org.au/about-bleeding-disorders/haemophilia
- Haemophilia Foundation Australia 2023c, Haemophilia Inheritance, Haemophilia Foundation Australia, viewed 29 January 2024, https://www.haemophilia.org.au/about-bleeding-disorders/haemophilia/haemophilia-inheritance
- Healthdirect 2023, Haemophilia, Australian Government, viewed 29 January 2024, https://www.healthdirect.gov.au/haemophilia
- Healthdirect 2020, Von Willebrand Disease, Australian Government, viewed 29 January 2024, https://www.healthdirect.gov.au/von-willebrand-disease
- The Royal Children's Hospital Melbourne 2013, Haemophilia, RCHM, viewed 29 January 2024, https://www.rch.org.au/clinicalguide/guideline_index/Haemophilia/
 New
New