Appendicitis is a serious condition with the potential to cause death, yet, it’s problematic to diagnose and has no proven way of being prevented (Emergency Care Institute 2023; Healthdirect 2023).
Therefore, being able to recognise the signs of potential appendicitis and escalate care appropriately is crucial to all healthcare professionals.
What is Appendicitis?
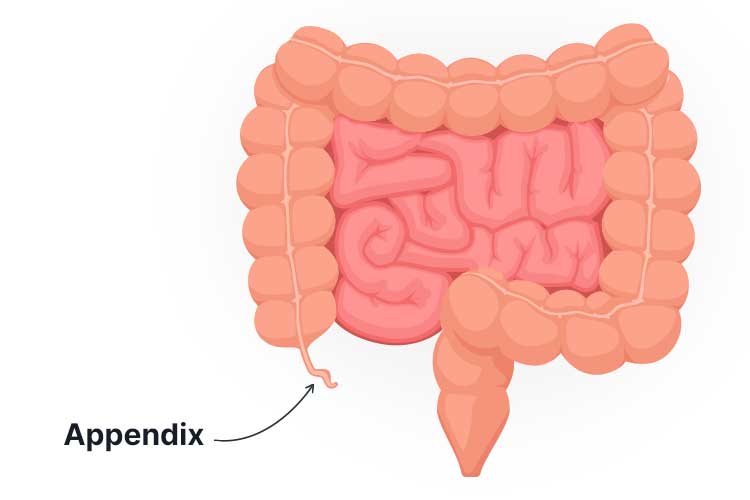
Appendicitis is an acute, potentially life-threatening medical emergency wherein the vermiform appendix (appendix) becomes inflamed (Jones et al. 2023).
The appendix is a thin, finger-like pouch that is attached to the caecum - a part of the large intestine located on the lower right side of the abdomen (Mayo Clinic 2023; Karunaharamoorthy & Mytilinaios 2023).
The exact purpose of the appendix in humans is still unknown - some believe that it functions as a lymphoid organ with immunoprotective properties, while others suggest its role is to store ‘good’ bacteria (Jones et al. 2023).
What Causes Appendicitis?
Appendicitis is generally thought to be caused by a blockage in the appendix, leading to acute inflammation and the multiplication of bacteria (Jones et al. 2023).
It’s not clear what exactly causes this blockage, but potential contributing factors include faecal matter, appendiceal tumours or swelling of the appendiceal tissue due to infection (NIDDK 2021; Jones et al. 2023).
The swelling and infection caused by appendicitis create increased pressure within the appendix. Eventually, this pressure will cause the appendix to rupture and spread its infected contents into the abdominal cavity, potentially leading to abscess or peritonitis (infection of the abdominal lining). This is an extremely serious complication that can be fatal without treatment (NHS 2022; Better Health Channel 2014; Mayo Clinic 2023).
The progression of appendicitis varies in duration, but generally, the risk of rupture tends to gradually increase after 36 hours from the onset of symptoms (Jones et al. 2023).
Risk Factors for Appendicitis
Appendicitis can affect anyone but most commonly occurs between the ages of 5 and 45 (Jones et al. 2023).
Males are slightly more at risk, with about 8.6% of males and 6.7% of females experiencing appendicitis during their lifetimes (Jones et al. 2023).
There also seems to be an increased risk among those who have a family history of appendicitis (Li et al. 2018).
Symptoms of Appendicitis

Appendicitis often begins with central abdominal pain near the navel that may come and go (NHS 2022).
Typically, the pain will eventually localise to the lower right quadrant of the abdomen, where it will become more intense and constant (Healthdirect 2023).
Touching or moving the stomach will generally exacerbate the pain (Healthdirect 2023).
Additionally, the patient may experience:
- Pain when walking or coughing
- Fever
- Nausea and vomiting
- Loss of appetite
- Diarrhoea or constipation
- Abdominal swelling
- Urinary frequency or urgency.
(Healthdirect 2023; Jones et al. 2023; Mayo Clinic 2023)
If the appendix ruptures, a significant worsening of symptoms and collapse will generally result (Better Health Channel 2014).
How is Appendicitis Diagnosed?
Appendicitis has several differential diagnoses, including, but not limited to:
- Gastroenteritis
- Ectopic pregnancy
- Crohn’s disease
- Urinary tract infection
- Ovarian torsion
- Ruptured Graafian follicle
- Kidney stones
- Meckel diverticulitis
- Intussusception (in children)
- Peptic ulcer disease
- Pelvic inflammatory disease
- Other infections (adenitis, peritonitis, cholecystitis).
(Abercrombie et al. 2023)
These differential diagnoses can make appendicitis difficult to firmly diagnose. It’s particularly tricky to diagnose in children, as they aren’t able to articulate their pain and symptoms as well as adults can (Healthdirect 2023).
Generally, the diagnostic process will involve physical examination and discussion with the patient about their symptoms. Medical imaging (ultrasound or CT scan) and blood tests might also be used, although they can’t give definite answers (Healthdirect 2023).
Due to the extremely serious nature of the illness and the need for timely intervention, surgery might be indicated even if the diagnosis isn’t clear (Healthdirect 2023).
Alvarado Score
The Alvarado score (MANTRELS) is a validated assessment tool designed to assist in the diagnosis of appendicitis:
| Symptom | Score |
|---|---|
| M - Migration of pain to the lower right quadrant of the abdomen | 1 |
| A - Anorexia (loss of appetite) | 1 |
| N - Nausea and vomiting | 1 |
| T - Tenderness in the lower right quadrant of the abdomen | 2 |
| R - Rebound tenderness (tenderness that occurs when pressure is placed on the lower right quadrant of the abdomen and then released) | 1 |
| E - Elevated temperature (fever) | 1 |
| L - Leukocytosis (high white blood cell count) | 2 |
| S - Shift of white blood cell count to the left (increased WBC count) | 1 |
(Emergency Care Institute 2023)
The patient’s score for each present symptom should then be added together:
| Total score | Interpretation |
|---|---|
| < 4 | Appendicitis is unlikely |
| 4 to 6 | Further imaging is required to determine whether appendicitis is present |
| ≥ 7 | Appendicitis is likely |
(Emergency Care Institute 2023)
How is Appendicitis Managed?
According to the Emergency Care Institute (2023), the management pathway for suspected appendicitis in non-pregnant patients is to:
- Resuscitate the patient if they are initially unstable (this is generally not the case unless the appendix has already ruptured, however)
- Consider differential diagnoses
- Undertake a thorough assessment if the patient is stable
- Perform medical imaging if appendicitis is suspected but still unclear
- Provide supportive care, i.e. nil by mouth, intravenous fluids and analgesic medicines
- Perform an appendectomy.
What is Appendectomy?

Appendectomy is a surgical procedure wherein the appendix is permanently removed. As the appendix is not essential for health, the body is still able to function normally with no noticeable changes after the procedure (Healthdirect 2023).
The appendix can be removed through either laparoscopic (keyhole) surgery or a small open incision made in the lower abdomen. If the appendix has already ruptured, pus will be drained from the abdominal cavity and antibiotics will be given intravenously (Better Health Channel 2014).
Appendectomy is generally the first-line treatment method for appendicitis. Antibiotic therapy can be used as an alternative treatment, but it’s less reliable and is generally only used alone if the patient is too frail to undergo surgery (Better Health Channel 2014).
The length of the postoperative recovery period will depend on the patient’s overall health, the type of surgery performed and whether or not the appendix had ruptured (Healthdirect 2023).
Test Your Knowledge
Question 1 of 3
Appendicitis characteristically causes pain in which area of the abdomen?
Topics
References
- Abercrombie, J et al. 2023, Acute Appendicitis: Differentials, BMJ Best Practice, viewed 9 January 2024, https://bestpractice.bmj.com/topics/en-gb/3000094
- Better Health Channel 2014, Appendicitis, Better Health Channel, viewed 9 January 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/appendicitis
- Emergency Care Institute 2023, Acute Appendicitis, New South Wales Government, viewed 9 January 2024, https://aci.health.nsw.gov.au/networks/eci/clinical/clinical-tools/abdominal-emergencies/acute-appendicitis
- Healthdirect 2023, Appendicitis, Australian Government, viewed 9 January 2024, https://www.healthdirect.gov.au/appendicitis
- Jones, MW, Lopez, RA & Deppen, JG 2023, ‘Appendicitis’, StatPearls, viewed 9 January 2024, https://www.ncbi.nlm.nih.gov/books/NBK493193/
- Karunaharamoorthy, A & Mytilinaios, D 2023, Cecum and Vermiform Appendix, Kenhub, viewed 9 January 2024, https://www.kenhub.com/en/library/anatomy/cecum-and-vermiform-appendix
- Li, H, Yeh, L, Huang, Y, Hsieh, M, Yu, K & Kuo, C 2018, ‘Familial Risk of Appendicitis: A Nationwide Population Study’, The Journal of Pediatrics, vol. 203, pp. 330-335, viewed 9 January 2024, https://www.jpeds.com/article/S0022-3476(18)31046-1/fulltext
- Mayo Clinic 2023, Appendicitis, Mayo Clinic 2021, viewed 9 January 2024, https://www.mayoclinic.org/diseases-conditions/appendicitis/symptoms-causes/syc-20369543
- National Health Service 2022, Appendicitis, NHS, viewed 9 January 2024, https://www.nhs.uk/conditions/appendicitis/
- National Institute of Diabetes and Digestive and Kidney Diseases 2021, Symptoms & Causes of Appendicitis, U.S. Department of Health and Human Services, viewed 9 January 2024, https://www.niddk.nih.gov/health-information/digestive-diseases/appendicitis/symptoms-causes
- Sepsis Alliance 2021, Appendicitis, Sepsis Alliance, viewed 14 January 2022, https://www.sepsis.org/sepsisand/appendicitis/
 New
New 
