Changes were introduced to the National Cervical Screening Program in December 2017 as a result of improvements in science, technology and research into how cervical cancer develops.
The primary change was that the cervical screening test replaced the procedure known as the Pap test (DoHAC 2022).
Cervical cancer is one of the most preventable cancers. Routine cervical screening is the best method of protecting oneself against cervical cancer. Avoiding the cervical screening test or being tested less frequently than recommended is a risk factor for developing cervical cancer (DoHAC 2022; Cancer Australia 2022).

What is the Cervical Screening Test?
The cervical screening test is a safe, quick test that can be performed in a few minutes by a doctor, nurse, women’s health centre, community health clinic or Aboriginal health worker in a clinic or consulting room (NSW Government n.d.).
The test is expected to protect almost 30% more people from cervical cancer than the Pap test was able to (DoHAC 2022).
People who have a cervix and are aged 25 to 74 are eligible for the cervical screening test. The cervical screening test is more accurate than the Pap test as it is able to detect the presence of human papillomavirus (HPV), a sexually transmitted infection that is the cause of 99% of cases of cervical cancer (Healthdirect 2022).
It is necessary to undergo the cervical screening test every five years rather than every two years, as was recommended for the Pap test (Healthdirect 2022).
It usually takes 10 to 15 years for abnormalities caused by the HPV virus to develop into cancer (Healthdirect 2022).
Even if a person has been vaccinated against HPV, they still need to take the cervical screening test. This is because the HPV vaccine protects people from certain strains of HPV that cause cancer, but not all (Queensland Health 2018).
What is Human Papillomavirus?
HPV is a very common virus spread through skin-to-skin contact. Generally, HPV does not have symptoms, though it can cause genital warts (Healthdirect 2022).
It's possible to contract HPV the first time you have sex, even if a condom is used. There are over 100 strains of HPV, and four out of five people have at least one kind of strain of the virus at some point in their lives (Healthdirect 2022).
Who Should Take the Cervical Screening Test?
People who:
- Have a cervix
- Are 25 to 74 years of age, and
- Have ever been or are currently sexually active.
(Healthdirect 2022)
The cervical screening test is necessary for people who fit these criteria, even if they have been vaccinated against HPV or if they identify as lesbian or trans gender (Healthdirect 2022).
What to Expect From the Cervical Screening Test
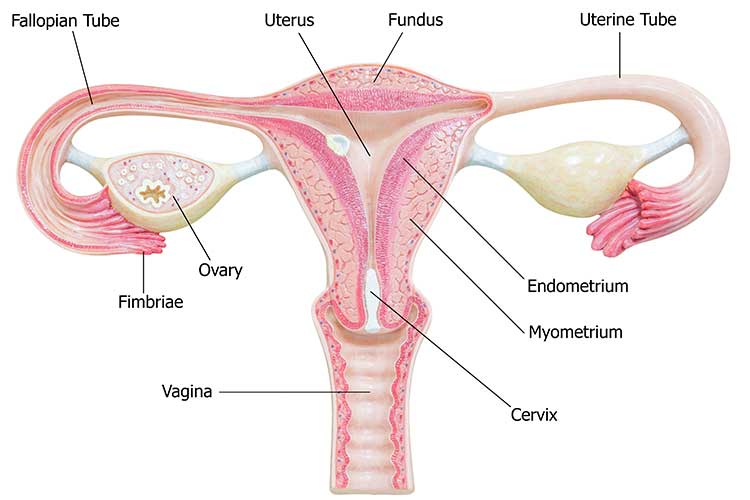
The test is a simple procedure to check the health of a person’s cervix (the entrance to the uterus from the vagina). It is performed in a private room in which the test will be explained to the patient by a nurse or doctor.
The procedure requires the removal of the individual’s clothing from the waist down. The patient should lie down on a bed with their knees bent and apart. The doctor or nurse will then gently insert a speculum into their vagina to keep it open and allow them to see the cervix (NSW Government n.d.).
A small brush will be used to take a sample of cells from the cervix. This procedure is often described as uncomfortable, but it should not cause pain (Queensland Health 2018).
The sample is put into a sterile tube and sent to a laboratory to be examined. A doctor will then discuss the results with the patient (which should take about two weeks to come through), which may reveal:
- The patient does not have an HPV infection: In this case, they will not need another cervical screening test for another five years, and they will be sent a reminder to do so by the National Cervical Screening Program.
- The patient does have an HPV infection: It is likely their body will get rid of the HPV on its own. They will need another cervical screening test in 12 months' time. It takes approximately 10 to 15 years for cervical cancer to develop. If the second test is clear, they won’t need another test for five years. If they still have the HPV infection after 12 months, they may be instructed to see a specialist.
- The patient has a certain type of HPV or an abnormality is found: A doctor will refer them to a specialist for further tests; this doesn’t necessarily mean cancer is present.
- The test result is unsatisfactory: This occurs if the sample could not be read at the laboratory. It will be necessary to repeat the test in 6 to 12 weeks.
(Healthdirect 2022)
Remember, while the procedure is uncomfortable and not something that people generally look forward to, these few moments of discomfort could be life-saving.

Test Your Knowledge
Question 1 of 3
True or false: 18 is the age that a person should first undergo a cervical screening test.
Topics
References
- Cancer Australia 2022, Cervical Cancer, Cancer Australia, viewed 16 January 2023, https://www.canceraustralia.gov.au/cancer-types/cervical-cancer/overview
- Cancer Institute NSW n.d., What Happens at a Cervical Screen?, New South Wales Government, viewed 16 January 2023, https://www.cancer.nsw.gov.au/cervical-screening-nsw/your-cervical-screening-appointment/what-happens-at-a-cervical-screen
- Department of Health 2022, About the National Cervical Screening Program, Australian Government, viewed 16 January 2023, https://www.health.gov.au/our-work/national-cervical-screening-program/about-the-national-cervical-screening-program
- Healthdirect 2022, Cervical Screening Test, Australian Government, viewed 16 January 2023, https://www.healthdirect.gov.au/cervical-screening-test
- Queensland Health 2018, Everything that Happens During Your Cervical Screening Test Appointment, Queensland Government, viewed 16 January 2023, https://www.health.qld.gov.au/news-events/news/everything-that-happens-during-your-cervical-screen
 New
New 
