Despite seeming similar, the terms ventilation and oxygenation relate to two separate (albeit interdependent) physiological processes. Understanding the difference between the two is critical in being able to effectively treat patients and make appropriate clinical decisions.
When confronted with a patient who is having respiratory difficulties, it is important to know whether they need help ventilating (getting air in and out of their lungs) or if they need oxygen due to hypoxaemia (impaired gas exchange).
Early detection of respiratory decline reduces the incidence of medical emergencies, the need for mechanical ventilation and the need for intensive care unit admission. Therefore, having adequate knowledge about respiratory anatomy and physiology means you will be able to respond to patients correctly and hopefully prevent deterioration (Vincent et al. 2018).
What is the Difference Between Ventilation and Oxygenation?
Ventilation
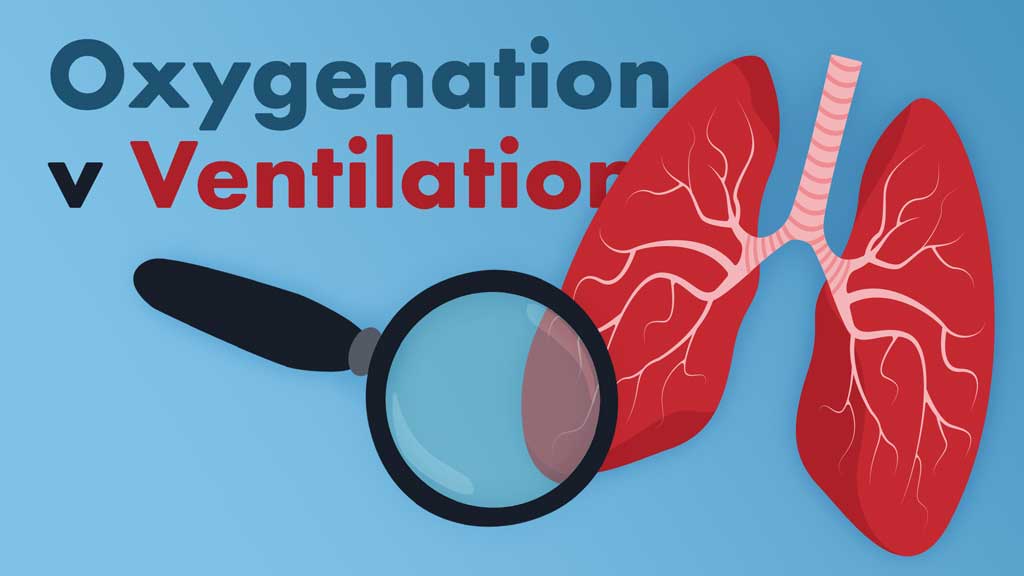
Ventilation can be considered the act of normal, spontaneous breathing. It refers to the two processes of inspiration and exhalation, i.e. the movement of air in and out of the lungs. (Pandirajan 2023).
These processes form a delivery system that provides the alveoli with oxygen-rich air (Dezube 2023).
Inspiration is initiated by the contraction of the inspiratory muscles (diaphragm and external intercostal muscles), which increases the volume of the thoracic cavity and, subsequently, the lungs. This creates a negative pressure that allows air to be easily drawn into the lungs (Pandirajan 2023).
Expiration is the opposite process, wherein the inspiratory muscles relax and cause the volume of the thoracic cavity and lungs to decrease. This creates a positive pressure that forces the air to move out of the lungs (Pandirajan 2023).
Ventilation can be measured by assessing clinical signs (chest rise, compliance and respiratory rate) (MedicTests 2019).
Oxygenation
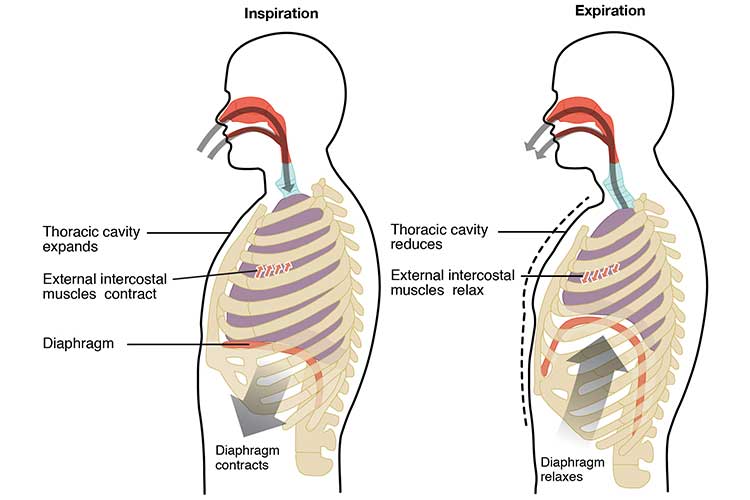
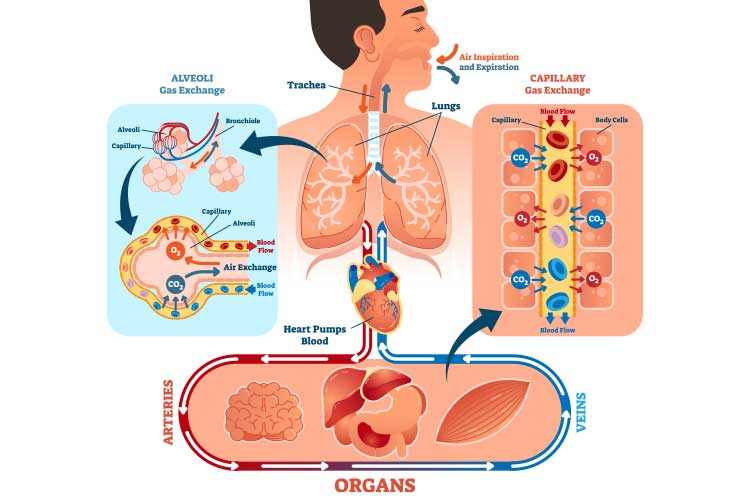
Oxygenation is the delivery of oxygen to the tissues to maintain cellular activity (MedicTests 2019).
It is part of the gas exchange process, wherein oxygenation occurs simultaneously with the elimination of carbon dioxide from the bloodstream to the lungs (Dezube 2023; Kaynar 2024).
These gases (oxygen and carbon dioxide) are transported through passive diffusion across the membrane, meaning the gas exchange process requires no energy expenditure from the individual (Dezube 2023).
Oxygenation can not be measured by assessing clinical signs alone; it generally requires a pulse oximeter (MedicTests 2019).
Respiratory Failure
Understanding the difference between ventilation and oxygenation is crucial when managing a patient experiencing respiratory failure, which is caused by an inability to maintain blood oxygen levels (hypoxia), an excessive amount of carbon dioxide in the blood (hypercapnia) or both at once (McKechnie 2024; MedlinePlus 2024).
There are four types of respiratory failure:
- Type I (hypoxaemia), an oxygenation issue causing low oxygen and normal to low levels of carbon dioxide
- Type II (hypercapnia), a ventilation issue causing low oxygen and high levels of carbon dioxide
- Type III (perioperative)
- Type IV (shock).
(Mirabile et al. 2023; Cleveland Clinic 2023)
In order to appropriately respond to a patient, you need to determine the kind of difficulty they are facing.
Type I Respiratory Failure (Hypoxaemia)
Type I, also known as hypoxaemic respiratory failure, occurs when an individual is unable to oxygenate adequately. It is clinically defined by an arterial oxygen tension (PaO2) of less than 60 mmHg (on room air). Carbon dioxide levels are normal or low. It is the most common type of respiratory failure (Kaynar 2024).
Type I is generally associated with acute lung diseases that cause fluid or sputum to occupy the alveoli (oxygen cannot swim through fluid or infection) or collapse of alveolar units (Kaynar 2024).
Oxygen therapy is generally required to treat patients with hypoxaemia (Mirabile et al. 2023).
Causes of Type I respiratory failure include:
- Pulmonary oedema
- Pneumonia
- Pulmonary haemorrhage
- Atelectasis
- Pulmonary embolism
- Acute respiratory distress syndrome
- Chronic obstructive pulmonary disease (COPD)
- Pulmonary fibrosis
- Pneumothorax.
(Mirabile et al. 2023; Physiopedia 2024)
Symptoms of Type I respiratory failure include:
- Confusion
- Shortness of breath
- Irritability
- Tachycardia (abnormally fast heartbeat)
- Tachypnoea (abnormally rapid breathing)
- Cyanosis.
(Physiopedia 2024)

Type II Respiratory Failure (Hypercapnia)
Type II, also known as hypercapnic respiratory failure, occurs when there is excess carbon dioxide in the bloodstream. This is usually caused by hypoventilation, i.e. the patient is unable to ventilate adequately enough to draw in the amount of oxygen needed. This results in unbalanced gas exchange, causing carbon dioxide to accumulate (Patel et al. 2022; Jewell 2023).
It is clinically defined by an arterial carbon dioxide pressure (PaCO2) of over 50 mmHg and may occur along with hypoxaemia (Mirabile et al. 2023).
Ventilatory support (invasive or non-invasive, depending on the clinical situation) is generally required to treat patients with hypoxaemia (Mirabile et al. 2023).
Type II respiratory failure is caused by conditions that impede ventilation, such as:
- COPD
- Asthma
- Acute neuromuscular disease
- Drug overdose
- Poisoning
- Head and neck injuries
- Pulmonary oedema
- Adult respiratory distress syndrome.
(McKechnie 2024; Mirabile et al. 2023)
Symptoms of type II respiratory failure include:
- Headache
- Shortness of breath
- Confusion
- Decreased conscious state or unconsciousness
- Seizures
- Hand tremors.
(Brody 2024)
Hypercapnia is a medical emergency that can be fatal if untreated (Brody 2024).

Conclusion
Patients experiencing respiratory failure will require appropriate intervention. It is crucial to differentiate whether it is a ventilation or oxygenation issue and treat the patient accordingly.
Care must be escalated to the medical team in the event of deterioration, as early intervention is vital to ensure the risk of mortality is decreased and invasive ventilation (if needed) is minimised.
Test Your Knowledge
Question 1 of 3
What is the primary physiological difference between ventilation and oxygenation?
Topics
References
- Brody, B 2024, Hypercapnia (Hypercarbia), WebMD, viewed 2 May 2025, https://www.webmd.com/lung/copd/hypercapnia-copd-related#1
- Cleveland Clinic 2023, Respiratory Failure, Cleveland Clinic, viewed 2 May 2025, https://my.clevelandclinic.org/health/diseases/24835-respiratory-failure
- Dezube, R 2023, Exchanging Oxygen and Carbon Dioxide, MSD Manual, viewed 2 May 2025, https://www.msdmanuals.com/home/lung-and-airway-disorders/biology-of-the-lungs-and-airways/exchanging-oxygen-and-carbon-dioxide
- Jewell, T 2023, ‘Hypercapnia: What Is It and How Is It Treated?’, Healthline, 3 March, viewed 2 May 2025, https://www.healthline.com/health/hypercapnia
- Kaynar, AM 2024, Respiratory Failure, Medscape, viewed 2 May 2025, https://emedicine.medscape.com/article/167981-overview
- McKechnie, D 2024, Respiratory Failure, Patient, viewed 2 May 2025, https://patient.info/doctor/respiratory-failure
- MedicTests 2019, Assessment of Ventilation, Respiration, and Oxygenation (Breathing), MedicTests, viewed 2 May 2025, https://medictests.com/units/assessment-of-ventilation-respiration-and-oxygenation
- MedlinePlus 2024, Respiratory Failure, U.S. Department of Health and Human Services, viewed 2 May 2025, https://medlineplus.gov/respiratoryfailure.html
- Mirabile, VS, Shebl, E, Sankari, A & Burns, B 2023, ‘Respiratory Failure’, StatPearls, viewed 2 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK526127/
- Pandirajan, K 2023, Mechanics of Breathing, TeachMe Physiology, viewed 2 May 2025, https://teachmephysiology.com/respiratory-system/ventilation/mechanics-of-breathing/
- Patel, S, Miao, JH, Yetiskul, E, Anokhin, A & Majmundar, SH 2022, ‘Physiology, Carbon Dioxide Retention’, StatPearls, viewed 2 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK482456/
- Physiopedia 2024, Respiratory Failure, Physiopedia, viewed 2 May 2025, https://www.physio-pedia.com/Respiratory_Failure
- Vincent, J et al. 2018, ‘Improving Detection of Patient Deterioration in the General Hospital Ward Environment’, Eur J Anaesthesiol., vol. 35 no. 5, viewed 2 May 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5902137/
 New
New