In order to accurately and correctly assess a patient using 5-lead monitoring, it is necessary to understand how ECG works, know how to prepare the patient and be able to follow the standardised system for electrodes and their placements.
What is an Electrocardiogram (ECG)?
An electrocardiogram (ECG) is a non-invasive method of monitoring the electrophysiology of the heart (Mayo Clinic 2024).
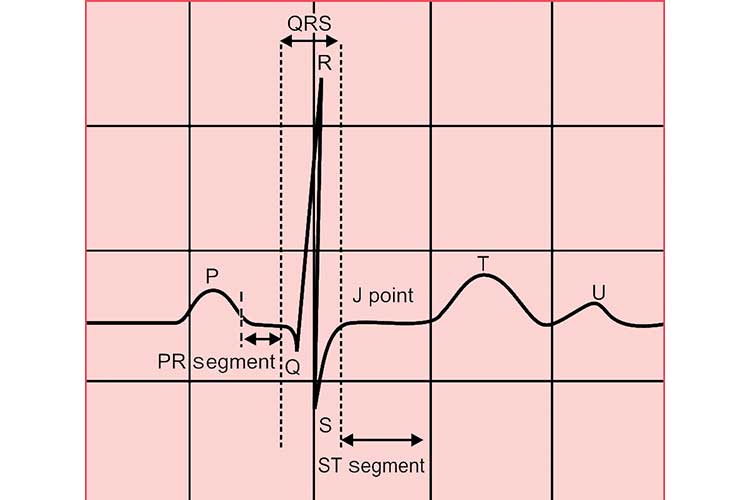
An ECG machine records changes in electrical activity by drawing on moving paper known as an electrocardiograph. The paper moves at a speed of 25 mm per second, and the ECG machine plots time on the x-axis and voltage on the y-axis. On the electrocardiograph, one second is represented by five large squares. These large squares are broken into five smaller squares, representing 0.04 seconds each. When the ECG machine plots the patient’s electrical activity, an increase of one mVolt in voltage moves the stylus by 1 cm (Sattar & Chhabra 2023).
While ECG is commonly used across a variety of medical settings, it plays a particularly important role in the haemodynamic assessment of intensive care unit (ICU) patients (Khan 2020).
All ICU patients generally require continuous ECG monitoring if clinically unstable. Continuous ECG monitoring can improve the detection of clinical deterioration (Khan 2020; Moss et al. 2017).
How Does an ECG Work?
An ECG involves the placement of electrodes onto the patient’s torso and/or limbs. The electrodes are connected to an electrocardiograph, which displays a pictorial representation of the patient’s cardiac activity (Better Health Channel 2023).
The waves detected and visually displayed through ECG illustrate the sequence of depolarisation (positive current) and repolarisation (negative current) generated by action potentials (electrical impulses) of the atria and ventricles in the heart (Klabunde 2023a).
In ICU settings, ECG is generally used for continuous monitoring of the patient’s heart rate and the detection of any potentially fatal cardiac abnormalities such as arrhythmias, but may also serve a diagnostic purpose (Sattar & Chhabra 2023).
What is 5-Lead ECG?
ECG measures the electrical activity of the heart from several leads (viewpoints) in order to construct a picture of the patient's cardiac function using voltage on the vertical axis against time on the horizontal axis (Cables and Sensors 2024).
Each lead has its own code name and represents the voltage difference between two electrodes. There are two types of leads:
| Lead type | Leads included | How they work |
|---|---|---|
| Bipolar leads (i.e. standard limb leads) | I, II, III | Measure the voltage difference between one positive electrode and one negative electrode. |
| Unipolar leads (i.e. augmented leads and chest leads) |
|
Have a single positive electrode and use a combination of the other electrodes as a composite negative electrode. |
(Cables and Sensors 2024; Klabunde 2023b)
Commonly used lead systems include:
- 3-lead monitoring, which uses 3 electrodes on the torso
- 5-lead monitoring, which uses 5 electrodes on the torso
- 12-lead monitoring, which uses 10 electrodes on the torso and limbs.
(Cadogan 2022)
12-lead monitoring is generally considered the standard form of ECG and provides the most information. However, it is not always feasible. Limb movement, tremor, anxiety and cold extremities may interfere with ECG readings, causing them to be of poor quality and consequently more difficult to interpret (Khan 2015).
As a result, torso leads are preferable as they allow for better quality ECGs. 3 and 5-lead monitoring take electrodes that are used for the limbs in 12-lead monitoring and instead place them on the chest wall in order to reduce artifacts (ECG signals that are from sources other than the heart) caused by patient movement (Khan 2015; Sampson 2018; Philips 2019).
5-lead monitoring is the same as 3-lead monitoring, but with two additional electrodes that enable the monitoring of extra leads and help improve ST elevation readings (Cables and Sensors 2024). It is able to monitor the leads I, II, III, aVR, aVL, aVF and V (Phillips 2019).
5-Lead Placement
Correct placement of electrodes is crucial.
The placement of electrodes for ECG monitoring is standardised to ensure that the information gathered is accurate and can be compared with records from other occasions. To ensure accurate results, the patient must also be correctly prepared both physically and psychologically (ADInstruments 2025).
Poor electrode placement can result in mistaken interpretation, which can lead to possible misdiagnosis, patient mismanagement and inappropriate procedures (Handzel 2023).
ECG electrodes are colour-coded, each identified by a specific code that refers to its intended placement. There are two coding systems currently in use:
- The American Heart Association (AHA) system
- The International Electrotechnical Commission (IEC) system.
Both systems are described in the table below.
| Location | Code (AHA) | Colour (AHA) | Code (IEC) | Colour (IEC) |
|---|---|---|---|---|
| Right arm | RA | White | R | Red |
| Right leg | RL | Green | N | Black |
| Left arm | LA | Black | L | Yellow |
| Left leg | LL | Red | F | Green |
| Chest | V | Brown | C | White |
(ADInstruments 2025; Cables and Sensors 2024; Cadogan 2022)
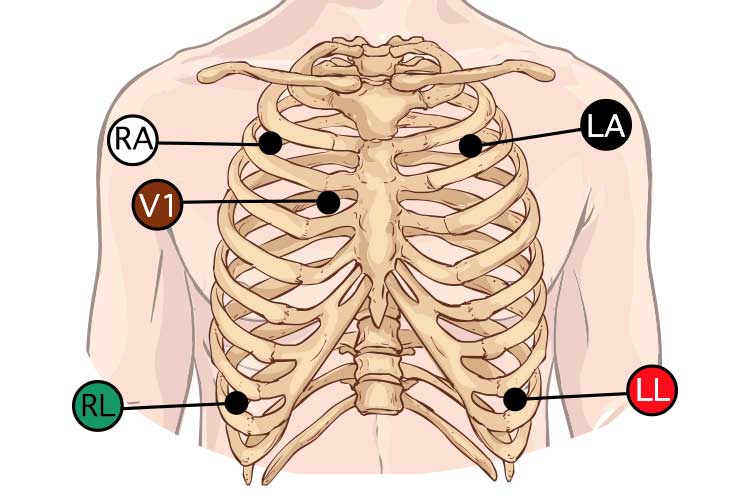
Method of 5-Lead Placement
Note: The following guide uses the AHA system.
- Prepare the patient physically and psychologically:
- Explain the procedure in detail.
- Obtain informed consent.
- Maintain patient dignity (i.e. give them privacy).
- Ensure the patient is in the supine position.
- Ensure the patient is comfortable and relaxed.
- Perform appropriate skin preparation:
- Select sites away from large muscle groups. Sites should be flat with intact skin.
- Dry, dead epidermal layers of skin should be removed. Natural oils and dirt should also be removed.
- Shave hair at the allocated sites.
- Wash sites thoroughly with soap and water. Rinse and dry well.
- Place the electrodes:
- The lead wires should be attached before the electrodes are applied.
- The electrodes should be applied by pressing around the edges instead of in the centre (this spreads the gel out and creates air pockets).
| RA placement | WHITE directly below the clavicle and near the right shoulder. |
| LA placement | BLACK directly below the clavicle and near the left shoulder. |
| RL placement | GREEN just below the right ribcage. |
| LL placement | RED just below the left ribcage. |
| V placement | BROWN on the chest - the position depends on your required lead selection (4th intercostal space, the right side of the sternum). |
- Connect lead wires to the ECG connector and ensure the waveform is visible on the monitor.
- Ensure all monitor alarms are on and audible.
- Always check with a colleague if unsure.
- Replace the electrodes at least daily, or more frequently as required.
(Elsevier 2024; Pope 2002)
Possible Complications
While 5-lead monitoring can provide an adequate amount of information, if something of concern is noted, such as a cardiac arrhythmia, 12-lead monitoring may be implemented in order to garner a better idea of the issue (Kleber 2022). Other investigations such as echocardiograms and blood tests may need to be considered.
Arrhythmias may cause haemodynamic instability, leading to loss of consciousness (Fletcher 2023). You should notify the medical team of any rhythm abnormalities and compare the patient with their previous 12-lead ECG (if one has been conducted).
Remember to always perform lead placement at the commencement of your shift as well as before and after repositioning the patient to ensure all electrodes and cables are in the correct position.
Test Your Knowledge
Question 1 of 3
In 5-lead ECG monitoring using the AHA coding system, where should the WHITE electrode be placed?
Topics
Further your knowledge
References
- ADInstruments 2025, ‘Correct 12 Lead ECG Placement for Researchers – A Simple Guide’, ADInstruments Blog, 5 March, viewed 29 April 2025, https://www.adinstruments.com/blog/correctly-place-electrodes-12-lead-ecg
- Better Health Channel 2023, ECG Test, Victoria State Government, viewed 29 April 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/ecg-test
- Cables and Sensors 2024, 12-Lead ECG Placement Guide with Illustrations, Cables and Sensors, viewed 29 April 2025, https://www.cablesandsensors.com/pages/12-lead-ecg-placement-guide-with-illustrations
- Cadogan, M 2022, ECG Lead Positioning, Life in the Fastlane, viewed 29 April 2025, https://litfl.com/ecg-lead-positioning/
- Elsevier 2024, Cardiac Monitor Setup and Lead Placement, Elsevier, viewed 29 April 2025, https://elsevier.health/en-US/preview/cardiac-monitor-set-up-and-lead-placement
- Fletcher, J 2023, ‘What to Know About Hemodynamic Instability’, Medical News Today, 29 March, viewed 29 April 2025, https://www.medicalnewstoday.com/articles/hemodynamic-instability
- Handzel, S 2023, ‘ECG Lead Misplacement: Looking at Common Issues’, Insights, 18 August, viewed 29 April 2025, https://www.gehealthcare.com/insights/article/ecg-lead-misplacement-looking-at-common-issues
- Khan, F 2020, ‘ECG in the ICU Patient’, in WJ Brady et al. (eds.), Electrocardiogram in Clinical Medicine, John Wiley & Sons, UK, viewed 29 April 2025, https://onlinelibrary.wiley.com/doi/epdf/10.1002/9781118754511.ch34?saml_referrer
- Khan, GM 2015, ‘A New Electrode Placement Method for Obtaining 12-lead ECGs’, Open Heart, vol. 2, no. 1, viewed 29 April 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4463488/
- Klabunde, RE 2023a, Electrocardiogram (EKG, ECG), Cardiovascular Physiology Concepts, viewed 29 April 2025, https://cvphysiology.com/Arrhythmias/A009
- Klabunde, RE 2023b, Electrocardiogram Leads, Cardiovascular Physiology Concepts, viewed 29 April 2025, https://www.cvphysiology.com/Arrhythmias/A013
- Kleber, K 2022, ‘5-Lead ECG Interpretation (Electrocardiogram) Tips for Nurses’, FreshRN, 11 November, viewed 29 April 2025, https://www.freshrn.com/5-lead-ecg/#12vs5
- Moss, TJ, Clark, MT, Calland, JF et al. 2017, ‘Cardiorespiratory Dynamics Measured from Continuous ECG Monitoring Improves Detection of Deterioration in Acute Care Patients: A Retrospective Cohort Study’, Plos One, viewed 19 April 2025, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0181448
- Mayo Clinic 2024, Electrocardiogram (ECG or EKG), Mayo Clinic, viewed 29 April 2025, https://www.mayoclinic.org/tests-procedures/ekg/about/pac-20384983
- Philips 2019, Improving ECG Quality, Philips, viewed 29 April 2025, https://www.documents.philips.com/assets/20191003/7d8c5dce56854cc9928baadb0178386a.pdf
- Pope, BB 2002, ‘How to Perform 3- or 5-lead Monitoring’, Nursing, vol. 32, no. 4, viewed 29 April 2025, https://journals.lww.com/nursing/Abstract/2002/04000/How_to_perform_3__or_5_lead_monitoring.38.aspx
- Sampson, M 2018, ‘Continuous ECG Monitoring in Hospital: Part 2, Practical Issues’, British Journal of Cardiac Nursing, vol. 13, viewed 29 April 2025, https://www.researchgate.net/publication/323523805_Continuous_ECG_monitoring_in_hospital_part_2_practical_issues
- Sattar, Y & Chhabra, L 2023, ‘Electrocardiogram’, StatPearls, viewed 29 April 2025, https://www.ncbi.nlm.nih.gov/books/NBK549803/
 New
New